One man's battle with Prostate Cancer-detailed

History of JC age 62 , first diagnosed at age 55 with a very rare and dangerously aggressive (only a 0.1% survival rate) form of prostate cancer. It did almost kill me (late in 2006).
This cancer is acting like "Small cell anaplastic androgen-independent neuroendocrine prostate cancer" (the cancer cells themselves are anaplastic and neuroendocrine, i.e. poorly differentiated).
Last names are omitted and other identifiers made vague (due to identity theft concerns). This is essentially a detailed diary of what I went through in this tough battle with this very dangerous form of cancer.
Last updated 03/15/2013
DISCLAIMER: I am not a medical professional in any way, just a victim of cancer.
I really welcome your comments after reading this blog (click on "comments" at the bottom of this web page to view or post your comment).
Of course, I also welcome your email. You can easily email me by clicking here: marcollins3040@gmail.com
Latest Update: click HERE for the latest details
3/15/2013-Rough day
3/14/2013-Back at hospice
3/7/2013-Still at home
3/5/2013-In home hospice care
2/10/2013-In the hospital
2/4/2013-Much has happened
2/1/2013-Radition and a transfusion
01/17/2030-Had chemo today
1/13/2013-Went to the ER
1/08/20102-Latest news
01/03/2013-Much has happened
12/20/2012-3rd dose of radiation and 4 blood tests
12/19/2012-much has happened
12/11/2012-Met with radiation oncologist
12/4/2012-Met with the oncologist, chemo postponed and mri scheduled.
11/28/2012-met with Oncologist and got CBC blood work
11/21/2012-Had the new drugs plus Aloxi for nausea
11/19/2012-Cancer 'significantly worsened' and I am switching to two chemo drugs
11/08/2012-Lupron today and cbc etc
10/25/2012-Zometa today
10/1/2012-MDV3100 Arrived
9/11/2012-Chemo change and CBC results
9/8/2012-went for a trip, had blood work done
8/22/2012-CBC blood tests, chemo next week
8/09/2012-I had chemo today and felt weird afterwards
7/26/2012-I had chemo today and felt bad afterwards
7/25/2012-much has happened
7/18/2012-CBC, MRI, Petscan
7/12/2012-no chemo this week. CBC blood counts too low
7/5/2012Chemo Today and zometa
7/3/2012-CBC, CMP blood test today
6/28/2012-Chemo today
6/21/2012-Chemo today
6/14/2012-Chemo today, blood test yesterday
6/7/2012-Received chemo today
5/30/2012-Met with oncologist and chemo is on for next week
5/22/2012-Met with oncologist and we have a plan now
5/9/2012-Met with oncologist today
5/3/2012-PSA came back
5/2/2012-Petscan results, blood tests, next steps
4/26/2012-Got a shot of neulasta today
4/25/2012-Saw oncologist yesterday, received chemo today
4/18/2012-Got the okay for taking 81 mg aspirin
4/17/2012-Saw oncologist today
4/10-13/2012-A lot has happened
4/3/2012-zometa today
3/15/2012-Chemo today
3/7/2012-PSA
3/6/2012-Met with oncologist and had CBC,CMP, PSA, PTT tests, zometa given also
2/29/2012-Oncologist postponed chemo and dental work due to blood chemistry issues
2/24/2012-Dentist visit and oncologist visit with CBC, CMP and PSA bloodtests
2/15/2012-went for chest x-ray, cbc and doctor visit
2/10/2012-Went to Dentist today
2/09/2012-Updated CBC
2/8/2012-MUGA REST today, details.
2/7/2012-Meeting with oncologist today
2/6/2012-My oncologist called me on Sunday
2/2/2012-Back at the hospital....
1/31/2012-Biopsy today
1/28/2012-CBC blood test results posted
1/25/2012-Biopsy scheduled
1/16/2012-Nutrient density of various foods
1/13/2012-met with oncologist etc
1/6/2012-medical update (lupron, chemo)
12/20/2011-double dose of colace worked fine
12/19/2011-Had a CBC today
12/16/2011-the day after chemo and 3 days after STRT
12/15/2011-Had cbc blood test and then chemo and zometa today
12/14/2011-Had the Sterotactic Radiotherapy (STRT) yesterday and met with my oncologist. Diet update also.
12/8/2011-Taking 2 percocet per day now
12/7/2011-PSA is 17
12/6/2011-lots of activity today and more to come
12/2/2011-met with Radiation Oncologist today & had an ultrasound exam.
11/29/2011-had an MRI last night
11/28/2011-Pain is back from cancer
11/10/2011-PSA came back at 12.5
11/8/2011-Blood test, lupron, port flush
10/15/2011-SPEAKUP
10/14/2011-Petscan results
10/13/2011-PSA is 9.1, platelets are 116 and I got a petscan today
09/30/2011-monthly update
08/24/2011-Kelly Eidem, Johanna Budwig
08/11/2011-flushed ports, visited Dr, received lupron.
07/13/2011-Blood test and lupron
6/14/2011-blood test from june 7th
5/26/2011-Chemo today and then a petscan and then one unit of blood
5/19/2011-Chemo today and one unit of blood also
5/17/2011-Blood test and wbc is normal now!
5/06/2011-Got a shot of neulasta today
5/05/2011-Chemo today
5/02/2011-2 units of blood given
4/28/2011-Blood tests, Chemo given and a plan for Monday also
4/25/2011-Blood test again and a dose of Neupogen given
4/21/2011-A major update
4/14/2011-More blood tests and I get my bone marrow biopsied.
4/6/2011-had blood test yesterday
3/31/2011-3rd round skipped due to blood chemistry
3/24/2011-2nd round skipped due to blood chemistry
3/17/2011-Clinical Trial started, first round of chemo given
3/15/2011-Another Clinical Trial
3/14/2011-MRI results
3/11/2011-MRI today
3/10/2011-cat scan, bone scan shows cancer
3/8/2011-florida, bone scan, cat scan lupron etc
2/5/2011-blood chemistry and lupron shot
1/27/2011-latest blood chemistry
1/21/2011-New transfusion (of red blood cells this time)
1/18/2011-new blood test results
1/14/2011-platelets falling again
1/10/2011-platelets rising!
1/6/2011-Another transfusion of platelets
1/3/2011-Major update - transfusion needed due to low platelets
12/8/2010-major update again
11/26/2010-major update
11/16/2010-todays tests etc
11/15/2010-More blood tests, a port and luj591
11/4/2010-2days of blood tests (CBC)
10/27/2010-minor surgery on my foot; targeted therapy to start soon
10/20/2010-Zometa Today
10/12/2010-Lots of information today
10/09/2010-petscan changed to 10/8 and ...
09/28/2010-next petscan/lupron is 10/12
09/09/2010-lupron and petscan
08/03/2010-Meeting with Oncologist
07/30/2010-Petscan yesterday - good news
07/13/2010-I fell on Sunday and wow!
07/08/2010-met with oncologist
07/06/2010-Read me: Updates to budwig diet and also green tea
06/03/2010-Lupron today
05/26/2010-Met with oncologist yesterday
05/20/2010-Met with Oncologist today
05/18/2010-Pet Scan results
04/26/2010-Colonoscopy
03/12/2010-More trouble
03/03/2010-Met with the oncologist.
02/26/2010-Pet scan results
02/15/2010-Hearing test today
02/12/2010-Met with neuorologist and oncologist
01/10/2010-Likely next step
01/05/2010-I am past the side effects of the chemo
12/21/2009-petscan and round 4 is next week
12/09/2009-Round 3 of chemo almost over
12/04/2009-Receive H1N1 flu shot today
11/30/2009-Home from the hospital
11/25/2009-I have shingles - UGH
11/24/2009-Side effects from chemo continue
11/22/2009-More good cancer news
11/18/2009-I feel normal today yet I have lost most of my hair
11/15/2009-Zofran drug is good and bad
11/12/2009-Round 2 is over with
11/10/2009-Day 1 of 2nd round of chemo & Flu shot today
11/05/2009-My hair is starting to fall out
10/30/2009-What procedures cost
10/27/2009-Met with the oncologist
10/26/2009-Chemo side effects are likely behind me now
10/22/2009-3rd day was a little different
10/21/2009-2nd day of chemo regimen just completed
10/13/2009-talked with the oncologist and we have a plan
10/12/2009-Petscan, Bonescan, Pain in left shoulder and more
09/24/2009-met with the oncologist on 9/22
09/02/2009_zometa and psa results
08/27/2009-Met with Oncologist and a Retina specialist today
07/31/2009-Research study results are in
07/28/2009-another research study
07/23/2009-Met with my medical oncologist
07/19/2009-Bone Scan results
07/13/2009-Had a bone scan today
07/09/2009-Petscan was yesterday and I have the results.
06/30/2009-Petscan scheduled and related comments
06/23/2009-Met with doctors today
06/15/2009-Surgery update
05/29/2009-Met with my internist
05/13/2009-Met with oncologist yesterday and we have a plan
05/06/2009-More test results
04/10/2009-Bladder is clear of cancer
04/02/2009-Cancer may have returned!!!!
03/23/2009-My next petscan is coming up (on 3/31/09 at 10am)
12/18/2008-Latest Petscan Results
11/25/2008-Insomnia etc
09/17/2008-Met with medical oncologist yesterday
09/12/2008-It is official! No sign of cancer!
09/11/2008-I had another petscan today
08/19/2008-Next petscan is middle of September
08/05/2008-If you or a loved one has cancer, please read todays post
08/01/2008-met with two doctors yesterday
07/29/2008-I may be signing up for ways to compensate for encephalopathy
07/08/2008-Petscan confirms no sign of cancer - hoorah!
06/17/2008-Petscan results
06/12/2008-Next step, another petscan
05/22/2008-NYU testing results
05/07/2008-Neuropsychological testing at NYU
04/15/2008-Meeting with my oncologist
04/10/2008-Petscan results
03/29/2008-Upcoming tests
03/10/2008-Met with Neurologist and family doctor
02/18/2008-Dental visit, neurologist scheduled
01/08/2008-Petscan results!
01/05/2008-The next Petscan is Monday (1/7)at 10am.
12/5/07-Gall bladder is out
11/11-No real news
10/23-I met with the Laparscopic Surgeon re my gall bladder
10/20-Diet change that may beat cancer!!
10/18-Gallstones, Diabetes may result from Chemotherapy
10/17-Met with my oncologist yesterday
10/10-My pet scan results and more
9/24-Update on my stamina.
8/22-My friend send me a photo he took of me so it is on this web and you can see how I look, compared to how I looked on 11/25/2006.
8/13-Went to a wedding in Vermont
8/5-Some strangers think I look 10-20 years younger!
7/27-The MRI of my Brain shows no cancer - hooray - I am cancer free now!!
7/26-I had an MRI today of my brain
7/25-Blood chemistry results back and I visited my dermatologist. Brain MRI is next.
7/19-Visit with my family doctor.
7/18-Update on visits to doctors (4 so far, 1 more to go)
7/18-Updated links on 4/22/2007 as the URLs were moved.
7/12-Am I consuming too much sugar with my daily diet of fruit juices?
7/6-Weight restrictions, good news from CT/PetScan!
6/12-Update on meeting with medical oncologist
6/10-Side effects still with me and....
6/7-I went to NYC to see the Radiation Oncologist today
6/3-Today is NATIONAL CANCER SURVIVORS DAY!
5/30-I am done with Radiation therapy!! Also, I added more details on my to-do list on 4/22/2007 (see item 9). I also fixed some spelling errors as I found them throughout this blog.
5/29-Went to VT for the w/e but side-effects are still with me. Radiation ends this week.
5/23-Radiation side-effects are back!
5/20-Tried Aloe on my radiation burns and it works well!
5/18-Met with two doctors today, received Lupron injection etc
5/17-Added photo (see 10/3/2006) showing me getting a round of chemo
5/16-Latest update on radiation etc
5/8-saw urologist yesterday and radiation oncologist doctors also re pain
5/4-Added two good book recommendations. The pain I felt from radiation is slowly going away.
5/2-Added some imbedded links so you can navigate easier. For example, clicking on LATEST UPDATE (above) takes you to the latest update. That is just one example of an imbedded link.
5/2-Doctor said to stay home and take Flomax and drink fluids; updated stats re Foley catheter - I had one for 63 days (all in 2006).
5/1-It hurts to urinate after 15 days of radiation. Could it be the radiation?
4/30-Radiation Oncologist asked me to stop my healthy drink (4/4/06) until radiation is over.
4/29-This blog is long so I added a summary below here
4/29-Added a photo of my pedometer which I use to measure progress. Also read a true story about this great hospital.
4/26-See 11/25/2006 for a picture of me in the Emergency Room on that date.
4/26-12 days of Radiation; new resource guide on prostate cancer that I found
4/23-Pomegranate Juice is easy to find at a good price and is a very healthy drink as well.
4/20-Added full treatment plan for radiation, many images
4/15-Added image of the tumor from cat-scan image dated 2/21/07
4/13-I have had 3 days of radiation treatment thus far.
4/10-We met with Radiation Oncologist and received a revised plan
4/8-A quick review of this battle with (prostate) cancer
If you click on any image, it should expand automatically for you.
*This blog is in date order so all updates are appended to the bottom of this blog, just so you know.
READ THIS PARAGRAPH CAREFULLY - the PSA test did NOT show any problems in my case so if I had relied solely on that, I would have died in the next 18 months or so. The Digital Rectal Exam is how they found it - Men - please do NOT rely solely on the PSA test!! Also if you have recently been diagnosed with Prostate Cancer and you live in the general NYC area (Long Island, NJ, CT, PA, NY), then contact me at "marcollins3040@gmail.com" asap and I will let you know the names of the doctor who treated me and where the surgery was. Then you can contact them also as needed.
THIS IS A QUICK SUMMARY OF WHAT I HAVE BEEN THROUGH
11/3/2005-1/16/2006-I am told I have prostate cancer and have to decide on the best course of treatment and the place to get treatment, i.e. the doctor and the hospital and the approach to take.
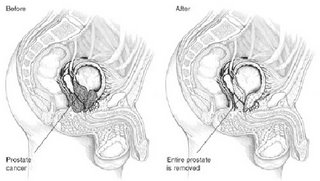
1/17/2006-3/5/2006-I have surgery (radical retropubic prostatectomy) on 1/17/2006 and recover during this period
3/6/2006-9/9/2006-I return to work and all seems well.
9/10/2006-10/2/2006-Cancer returns with a vengeance and a truly difficult period begins for me, i.e. bladder problems, left leg hurts, etc
10/3/2006-Chemo commences and I am having continuing major bladder problems (bladder spasms etc)
11/25/2006-I am losing far too much blood (50%?) due to bleeding in my bladder and am quickly hospitalized, yet again (4th time since 9/10); I likely lost 1/2 of my body's blood due to bleeding (and was getting light headed/dizzy from this). See photo below for date 11/25/2006.
12/1/2007-Chemo drugs NOT working, so new regimen of drugs start today.
12/5/2006-A surgical procedure forces my urine to largely bypass my bladder to give it a much needed rest. I finally go home 12/7/2006
12/14/2006-My foley catheter is removed and this is the last day of having one (thus far)
12/16/2006-I awake to major pain in my right flank. We rush to an ER and they find nothing at this time
1/30/2007-I develop a urinary tract infection requiring a visit to an ER
2/8/2007-Final round of new regimen of drugs today. The drugs really have hit me hard!
2/13/2007-My bladder is put back to work full time and it works well!!
3/23/2007-I return from a week in Florida and feel much better; no more naps needed as one example. We meet with a radiation oncologist as radiation 'could be my home run' in beating cancer.
3/27/2007-Orthopedic doctor tells me I can walk or swim but no sports or treadmill for the rest of my life. I am also not allowed to lift more than 25 lbs - all due to cancer damaging my left hip.
4/11/2007-IMRT Radiation commences today and will run about 5-6 weeks.
6/7/2007-IMRT Radiation ended on May 29th 2007 but the side effects do linger.
7/27/2007-Numerous tests (Bone Scan, Pet Scan, MRI) show no sign of cancer so I am now officially in remission.
10/16/2007-Petscan (10/3) still shows no sign of cancer but now I need gall bladder surgery (on 11/28).
04/2009-Cancer returns in my abdomen
06/09/2009-I have that cancer removed surgically
07/2009-Bone scan shows two hot spots - cancer comes back again
12/2009-Chemo resumes again
5/17/2010-Petscan shows 4 hot spots now
7/30/2010-Petscan shows one hot spot now
Recap of period 9/10/2006-1/30/2007:
* I lost some 20% of my body weight (between 9/10/2006 and year end 2006)
* I had some 7 Emergency Room visits (between 9/10/2006 and 1/30/2007) in three different hospitals in two different states.
* In all, I spent some 24 days in the Hospital (1/1/2006-12/7/2006, 20 of which were unscheduled.
* I had some 15 days of chemotherapy via IV Infusion (9/10/2006 through 2/8/2007)
* I had countless X-rays (15?), blood tests (50-75?)
* I had countless IV tubes put in me (40?)
* I had 4 cystoscopy procedures (since 9/10/2006)
* I was given 6 units of blood due to tremendous blood loss (11/25/2006).
* I am given countless doses of prescription drugs, some are quite expensive indeed!
* I have kidney tubes in me some 70 days.
* Some 73 days with a foley Catheter in me (14 planned days and the rest unplanned)
* Numerous tests: cat scans, pet scan, bone scans, MRI, Bone Density scan, X-Rays etc
* My spouse thought I would die by year end 2006 - that is how sick I was!! See the photo below on 11/25/2006 when I am admitted due to major blood loss.
Chemo and other events summarized
TAXOTERE/AVASTIN-10/3/06-11/30/06
CISPLATIN/ETOPOSIDE 12/1/06-2/8/07
KIDNEY TUBES USED 12/5/06-2/15/07
RADIATION THERAPY 4/11/07-/5/23/07
GALL BLADDER REMOVED 11/28/07
NYU DIAGNOSES CHEMO BRAIN 5/7/09
TUMOR REMOVED 6/15/2009
CISPLATIN/ETOPOSIDE 10/20/09-12/31/09
LUJ591 THERAPY 11/24/10-12/8/10
CARBOPLATIN/PACLITAXEL 3/7/2011
NAVILBLENE 11/21/11-5/19/11
ABIRATERONE/ZYTIGA oral 7/13/11
CABAZITAXEL/JETVANA 12/15/11-1/6/12
MITOXANTRONE 2/9/12
CISPLATIN/ETOPOSIDE reduced dose 6/7/12-8/16/2012
MDV3100 (oral) - scheduled for 9/28/2012
CYTOTAXON and VINCRISTINE-scheduled for 11/21/2012
TAXOTERE starting 1/17/2013
========The actual detailed history begins here=====
**This is of necessity detailed and long because it is my history**
**of all I have been through. It is well worth reading so many have**
**told me but expect it to take a while to read. I suggest you read a**
**bit each day and simply note the date you left off at so you can**
**resume later, as it is in date order.**
On 11/3/2005, I met with the family doctor (Dr. FrankM) for my annual routine physical and blood test. His only concern was he felt a lump on my prostate during the digital rectal exam. He otherwise stated I am fine. He then referred me to Dr. RichardG, a NJ Urologist. My blood test value of the PSA was 3.15, up from 2.54 in July 2005.
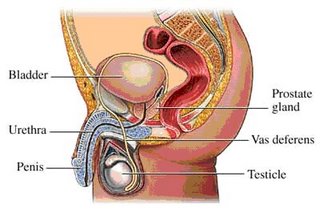
Sidenote: You can find a good explanation of the prostate gland at this url;
On 11/10/2005, I met with Dr. RichardG and he also did a digital rectal exam and concurred with Dr. FrankM and Dr. RichardG then recommended a biopsy to see what it might be. He cautioned there was about a 30% chance it is cancer.
On 11/29/2005, Dr. RichardG did the biopsy and took 12 tissue samples and sent off to the lab.
On 12/1/2005, Dr. RichardG. called me at work to say I have cancer and a high Gleason score (9). He immediately recommended a bone scan and a cat scan (with contrast) of my lower abdomen. When prostate cancer cells get loose in the body, they tend to head for the bones and joints and by then it is much harder to beat. Thus the request for a bone scan right away.
On 12/8/2005, these tests were done at a NJ area Hospital. I also asked for and received (via CDROM) copies of the bone scan/cat scan. I then drove to Dr. RichardG's office and also received copies of my biopsy. I noticed all 12 samples had some indication of cancer.
Side note-I started letting coworkers, friends, colleagues know that I had prostate cancer and one of the reasons (among many) is to see who they knew in my situation and what doctors, if any, they would recommend. That is how I found Dr. EDV (see 12/20/2005 notes) who is a GREAT doctor, actually writes textbooks on my problem and teaches at a well known medical school and is perhaps one of the best doctors for this problem in the entire country. He is also a caring human being.
On 12/13/2005, Dr RichardG asked to meet with me and my wife which we did this evening. He said the Bone Scan was clear and the CatScan found a 14-15mm lump in a lymph node which may be cancerous. (My family doctor concurred but said I could have had a lump like this for 30 years, i.e. not cancerous). So it needs to be proven somehow. Dr RichardG said I have an aggressive cancer with perineural invasion and we should go after it. If we go after it and remove it, statistically speaking, the cure rate is 20%-40% after 10 years and if lymph nodes are involved, it is much lower. He stated if I do nothing, I will be likely dead in 2-3 years. The surgery is called Radical Prostatectomy and is tentatively scheduled for mid-January at a major NJ Hospital.
He said it will then be followed with hormone therapy (pills/shots) to drive Testosterone levels in my body down to zero to kill rogue prostate cancer cells left in me) and my blood PSA will need to be monitored as it should then show a very low level, i.e. 0.0 to 0.1; he cautioned there may be microscopic cancers elsewhere in my body and thus no guarantees.
Also presented was a less aggressive approach of radiation consisting of seed implants, external beam radiation and hormone treatments.
Prostate cancer does not respond well to chemotherapy and radiation is not necessarily indicated as if it does not work, then he cannot do surgery due to scar tissue damage. He also cautioned that the prostate nerves might not be spared and I also will suffer a period of incontinence as well after the surgery. He also referred us to Dr. GlenG, clinical director of the Department of Radiation Oncology at XXX Medical Center) who I am meeting on December 27th at 3pm. Dr. RichardG also asked for an MRI (see 12/19 notes).
On 12/19/2005, I had a 2 hour MRI of my prostate (w/o GAD and with an Endorectal Coil) and Pelvic area at another NJ Hospital. This apparently is to get a better/clearer picture of my prostate and surrounding area. I met with family doctor (Dr FrankM) afterwards and we discussed (a) getting a 2nd opinion (b) likely surgically removing all cancer. I also started keeping notes on what I am going through and that is how this blog started - it helps me keep track of names, dates and so on and I hope it helps you.
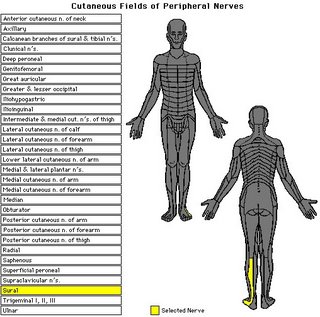
On 12/20/2005, I met with Dr. EDV, a senior doctor at a major NYC Hospital. He said I was dealt a bad roll of the dice and perhaps 10-15% of men get this kind of cancer. He said he can remove it and likely should. He can also get me into clinical trials after surgery. I asked about using the Sural nerve to replace nerves on the prostate and he said he would likely use the Genital Femoral nerve instead (it is closer and also less of an impact on me. Some details on the below link: (http://www.wheelessonline.com/ortho/genital_femoral_nerve)
On 12/21/2005, Dr. RichardG called and said the MRI apparently showed the cancer reasonably contained to the prostate. [The MRI was absolutely wrong, read on].
On 12/22/2005, Dr. KeithC of California (a college friend who is now director of surgery in California) called and said his team at their Hospital recommended surgery (“cut it out”), same as Dr RichardG and Dr EDV.
NOTE: This is not a reflection on the skill or compassion of Dr. RichardG who seemed very professional (and carefully hand-picked by Dr FrankM). I simply wanted a second option and Dr EDV is a renowned surgeon at a very good hospital (ranked the #1 in the tristate area). Hence, I switched to Dr EDV about this time.
On 12/27/2005, I met with Dr. GlenG, a radiation oncologist in NJ. If I am comfortable with surgery, he feels that is okay to do. He concurred one does not do radiation first and then surgery due to scar tissue. He offered that surgery may not get it all and the pathology report is also quite important. Dr. GlenG offered IMRT radiation may be called for after the surgery as some 50% of all men with prostate cancer develop other cancer later on and IMRT can reduce that. He also said IMRT has little side-effects. He said radiation can be used instead of surgery but that is up to me. He also commented on my high Gleason score, i.e. fairly aggressive cancer.
Note: this continues to get complicated, with a multitude of choices:
1-Surgery will remove 99+% of (capsule-confined) prostate cancer and it is considered major surgery and does have some significant side-effects.
http://www.prostate-cancer-institute.org/prostate-cancer-treatment/radical-prostatectomy.html
and http://www.upmccancercenters.com/cancer/prostate/radprostretropubic.html
2-External beam radiation can use IMRT techniques which uses highly focused radiation (guided by 3-D computed tomography (CT)) with some success and fewer side-effects (http://www.radiologyinfo.org/content/therapy/imrt.htm).
3-Brachytherapy uses radioactive seeds implanted in the cancer cells and kills them. More details found at http://www.brachytherapy.com/prost-brachy.html
4-Hormonal (endocrine) therapy – Androgen Ablation e.g. anti-androgens, medical castration (LHRHa) or surgical castration: http://www.marinurology.com/articles/cap/learning/hormonal.htm
5-There is also something called Ablatherm® HIFU (High Intensity Focused Ultrasound) to deal with prostate cancer (http://www.hifu.ca/home/index.php).
6-There is also Cyrotherapy which uses extreme cold to kill prostate cancer cells. (http://www.radiologyinfo.org/content/interventional/cryo.htm)
A good summary of most of the above choices can be found at this (and other) web sites: http://www.nci.nih.gov/cancertopics/understanding-prostate-cancer-treatment/allpages
Also, Michael Milken (Wall Street Junk Bond czar (Drexel Burnham Lambert)) developed prostate Cancer and founded this resource: http://www.prostatecancerfoundation.org/
Each approach has its advocates also, surgeons want to do surgery and radiation oncologists want to use radiation so it is for the patient (!) to decide what is best. But we do not have the education, skills or the experience to make an informed decision.
I thus placed a call to Dr. FrankM as why do we have to decide but he was unavailable at the time. He left a message that I am to decide what makes sense for me- this seems silly to me as I indicated, i.e. ordinary people do not have the training, education, skills or experience to make an informed decision. But all doctors appear to ask the patient to decide - weird!
There are numerous clinical trials underway for prostate cancer as found at the Cancer.gov web site: (http://www.cancer.gov/clinicaltrials/).
So why did I opt for major surgery?
1-The gleason score was 9 which indicated an aggressive cancer and actively attacking me. Had it been 1 or 2, I would have gone for watchful/waiting or radioactive seeds.
2-The Biopsy showed all 12 samples from my prostate to be cancerous. Thus it was fully engulfed.
So knowing it was aggressive and fully engulfing my prostate already, I opted for surgery so (1) they could cut it out and (2) while my abdomen was open, they could see how widespread the cancer was if it had moved beyond the prostate. That is why I chose surgery.
On 12/27/2005, KathyH of Dr EDVs office spoke with me and said to donate 1 pint of blood near the hospital approximately 1/9/2005 (in advance of surgery, now scheduled in NYC for 1/17/2006) and see her also at that time and Dr. EDV also. She also said to commence Ferrous Sulfate (325mg, 3xdaily) and Colace soon, i.e. now if I wish.
Ferrous Sulfate will increase the iron content in blood but is constipating hence the use of Colace, a stool softener. After surgery and when I am discharged from the NY Hospital, she said to bring loose fitting pants (not jeans) as I will have a catheter. She said to bring a pillow to sit on in the car for comfort during the ride home. The catheter will be a slim bag during the day and a bigger bag overnight. It stays in until 1/31/2005 when I see them again in NYC. She also said I am well be out of work for a total of 4 weeks.
On 12/28/2005, to insure biopsy was done accurately (and perhaps for other reasons), KathyH (Dr. EDV’s asst) asked me to have CBL send the original prostate biopsy slides to Dr. EDV. I contacted CBL, filled out a fax and sent it back to CBL for authorization to send them out to Dr. EDV. Once received by CBL, they will fed-ex them to Dr. EDV. They were scheduled to arrive on 1/3/2005.
KathyH called me to bring me up to date on a number of issues. Specifically, she recommends I give the unit of blood at 10:30am, not 1130am next Monday. So I switched this to 10:30am. This is not a fasting blood test so eat well if I wish before hand. After the blood donation, grab a lunch and then see Kathy for preadmission details and then the EKG etc at the NYC Hospital- I will be at the hospital for about 90 minutes in all.
For the Blood Donation at the NY Blood Center, walk in and state my file# is XXX and my patient # is XXXXX and then they will know me and what to do.
Regarding Colace and Ferrous Sulfate (Iron) pills, KathyH said I am to take a Colace pill with every Iron pill (both pills, 3 times per day) but do not take an Iron pill after breakfast on 1/16/2006. Colace and Iron pills resume when I am return home (through 2/1) and perhaps longer.
Also, as prep for surgery on 1/17/2006, KathyH said my last substantial meal is to be breakfast on 1/16/2006 and then clear liquids thereafter (No OJ, but Pomegranate is ok, as is clear chicken broths and so on). This includes lunch and dinner on 1/16/2006. No food whatsoever after midnight on 1/16/2006. I am expected to use the Fleet enema both on the evening of 1/16/2006 and the (early) morning on 1/17/2006 to clear out my intestines (likely due to the fact that intestines may shut down for a period of days after surgery).
I called KathyH back and she said to plan on being home for 3 weeks once I am discharged from the hospital.
This web page has another view of my surgery and thus offers another important opinion.
http://urology.jhu.edu/surgical_techniques/radical_prostatectomy/
http://www.radiologyinfo.org/content/mr_prostate.htm
MRI of the Prostate - normal exam. This view is looking up from the feet towards the head of the patient.
(A: right hip, B: bladder, C: left hip, D: prostate, E: rectum)

http://kidney.niddk.nih.gov/kudiseases/pubs/uimen/
Before:
After:
=========================================================================
Nerves that were discussed for possible grafting i.e. Sural nerve and Genitofemoral nerve
http://www.inletmedical.com/img/pgill/uplift_procedure_fig_i.jpg
Genitofemoral nerve location:
http://www.neuroguide.com/genitofemoral.html

==================================================
On 1/5/2006, KathyH emailed me that they received the biopsy slides and their pathology department is reviewing them. She also confirmed that Dr EDV has received the MRI report but has not commented on them as yet. I relayed my hopes that if he cannot save my nerves on the prostate (Nerve Sparing), then he will kindly graft other nerves to replace them. Regarding incontinence, she stated they do not have problems with stool/fecal incontinence. Re urinary incontinence, she recommended I exercise my Kegel muscles to reduce the chance of urinary incontinence. She also does not think I will go to the ICU after surgery – just to recovery and then a room. The timing of this depends somewhat on room availability. Re my anesthesia, she said I will be in morphine for a day or two and then Percocet and then Vicodin thereafter.
DickB at work told me that Dr. AndrewP is a good friend of his and was recruited from a major NYC Cancer Hospital to head the Cancer Center at XXX NJ Medical Center. He recommended I mention his name to anyone I use at the XXX NJ Medical Center.
Susan (my sister) called and said her former boss at the Scripps Clinic in San Diego was Dr. T and, by way of Susan, he strongly recommended I consult with Dr. MichaelZ at the Sloan Ketering Institute and was the #1 rated Radiation Oncologist in the entire world. So I called for him and he had left for the day and his assistant took my name (and Cell #) in hopes we can meet Monday Afternoon (she did not know his schedule for Monday). Apparently Mr & Mrs. SaleemD also recommended him.
On 1/9/2006, we went to NYC for a few reasons…specifically, I donated that pint of blood (see 12/27) at the NY Blood Center. Then we went over to the NYC hospital, first for lunch and then to see KathyH and Dr. EDV (briefly). Kathy gave us more instructions and also arranged for the blood test, the EKG and the Chest X-rays. We met up with Dr. EDV between the EKG and the Chest X-Rays for 30 minutes to discuss aspects of the surgery, preparation, prognosis etc. He felt it is confined to the prostate (based on the MRI) but likely microscopic prostate cells are elsewhere in my body as well. So we will use radiation and/or hormones and/or clinical trials to deal with it. There can be no nerve sparing but he will try to graft another (genitofemoral?) nerve in their place. He said radiation may be indicated after surgery and/or clinical trials. The MRI shows the cancer is not in the seminal vessels. Surgery should 2.5 hours or so and if scheduled for 730am, it may really start at 8am. I gave him clear direction that only my wife makes medical decisions if I am not able to and he said okay (my mom and two sisters would also be there and I wanted him to have clear direction). He also said if surgery runs longer than 2.5 hours, do NOT be alarmed. They may be grafting nerves etc. We were done talking around 5pm or so.
Among Kathy’s other comments on 1/9/2006:
* After surgery, drink a lot of water to drain the bladder into the catheter bag. The bag should never be empty per se, always draining.
* Expect the urine to be perhaps pink in the catheter bag (minor bleeding) but not darker.
* Sit-ups will help build my abdominal muscles and Kegel exercises now will be helpful also for incontinence control. Do these before surgery. After surgery, I may experience stress incontinence for a period of time, i.e. (coughing, getting up, laughing etc may trigger some urine drips).
* Seek help if temperature goes above 101 but I may have a low grade fever.
* I should have (and I did) stop taking aspirin and Vitamin E supplements by now.
* Take only MultiVitamin and Ferrous Sulfate/Colace and Lopid now. I should stop Ferrous Sulfate as outlined above, i.e. not after breakfast on 1/16/2006.
* My anesthesia will be by epidural as this is less stress on me and I will likely not go to an ICU after surgery, i.e. I will go from surgery to recovery and then to a room.
* She said to wear sweatpants at home to keep pressure off the incision and boxer shorts while I have the catheter.
Other sources (web pages) also said to apply gel to where the catheter exits to keep irritation down.
On 1/12/2006, KathyH referred my specimen request to pathology who said they (a) analyze them and (b) do not give specimens to patients. Regarding the catheter, she said they will provide instructions after surgery, i.e. Lidocaine and perhaps some lubricant. Pathology told me they will not release specimens to patients. Too bad – I planned to keep in a jar with formaldehyde and swear at it daily – to get even with it. I emailed Dr EDV asking he keep a small specimen for me. He replied and said he will try to get me the slides but cannot get a specimen for me – Pathology wants to keep it for research.
EdwardG, a fellow coworker, told me had prostate cancer (Gleason score 6) some 5 years ago and he had radiation and they think it worked for him, i.e. they cooked his prostate. He also said that Dr. ZviF of Memorial Sloan Kettering is a radiation expert.
My wife spoke with LesG, “he was diagnosed last February...had radiation…a Gleason score of 6"...I called him and we spoke for some time. He had originally planned surgery at Hackettstown hospital and then discovered they rarely did prostate surgery so he instead had radiation at Morristown Hospital. I explained I am choosing surgery because if I had a lower Gleason score and/or fewer positive biopsy hot spots, I would have chosen radiation. But with my score of Gleason 9 and 12 for 12 biopsy hot spots and a great doctor/hospital, I feel surgery is indicated for me and he concurred with me and wished me much luck.
On 1/16/06, we drove to Manhattan and checked into the Bentley Hotel; also there were my mother and sister Susan who flew in from Florida earlier in the day. We all went out to eat but I could not as I was told nothing after breakfast on 1/16/06. I also had to use a fleet enema both on the evening of 1/16 and early on 1/17 to clear out my rectum area. Tomorrow, my son will drive in with Charles (for the day) and my sister Ruthann will take a train down from upstate NY and stay a few days in NYC.
On 1/17/06 at 5:30am, we took a cab up to the NYC hospital and entered on 68st and went to the ‘G’ Pavilion (3rd floor) for same day surgery. There they hooked up two IV shunts, took my blood pressure, my pulse and my temperature. They also offered a health care proxy form which I signed, making my wife the decision maker if I was not conscious and they needed a decision. They then withdrew a vial of blood – they said they used that vial to match my blood from what NY Blood Center sent to insure it is one and the same (neat!). Then they had me change into gowns and walked me down a long hallway to Operating Room #3. It is now about 750am and was quite bright in there and I spotted 3-4 OR nurses standing along the back wall, two anesthelogists and a few other people. Dr. EDV then walked in with a student doctor and asked me if it was okay if the student doctor stayed and I said sure. They asked me to get up on the operating room table and lay down – then they gave me an epidural to numb me from the waist down; then they asked me to lay on my back and stretch out my arms which they then mildly restrained with towels or something - I asked why and they said in case I changed my mind about surgery! I am sure they also gave me another drug as I then became quite drowsy. The surgery was to last 2.5 hours but Dr. EDV said do not be concerned if it runs longer.
Sometime during surgery I was conscious of a face mask being placed on me, i.e. general anesthesia. I next woke up in a recovery area and spotted a clock and it said 1pm – I mildly panicked – why is it 5 hours later and now 2.5 or 3 hours later? I wondered. My recovery room nurse (IrmaS) said not to worry while she CLOSELY monitored me, i.e. my blood pressure every 90 seconds or so, my blood O2 level, my body temperature and so on – all continuously. They also had inflatable bags around my legs that kept inflating and deflating every 60 seconds (to move blood around and reduce the chance of clots. Irma after a while asked me if I felt my feet (I said no)…finally I did and could move them. She asked me to move my leg, i.e. lift it up, bending at the knee. The right leg went fine but the left leg did not work and she said this was normal – give it time. I was likely fully out of the effects of anesthesia by 5pm or so. While in the Recovery room, first my wife and my son visited me and then later my wife and Susan. My wife said I asked how many times I died on the operating room table – she also said I looked very pale – I vaguely recall that conversation. Irma also put my pint of blood back in me from NY Blood Center as they did not need it in surgery so they put it back in me via the IV shunt.
Note: The surgery ran 2 hours longer as the surgeon removed the cancerous prostate, a tricky procedure as it is VERY close to the bladder and rectum and so on. But he also then noticed there was some cancer on my bladder (both front and back portions) so he cut that out and then "reconstructed" my bladder. He also removed some nearby lymph glands that also appeared cancerous.
The surgery likely went something like this:
http://www.cornellurology.com/uro/cornell/prostate/treatments/prostatectomy.shtml
Irma fed me ice chips as needed and I was flat on my back for the rest of the day and night. Irma also said there was a shortage of beds in the hospital and she would try to find me one. By 11pm she finally found one and I was wheeled into the elevator and down a floor to a room on the 2nd floor on the north end of the building. I also had a Foley catheter in me as well as two surgical tubes in my lower abdomen draining excess fluids out of me. The surgical tubes were connected to a plastic device that looked like a pancake that wanted to expand. By trying to expand, it quietly created a partial vacuum that pulled fluids from my abdomen. Overall - I slept quite well that night.
On 1/18/06, they had me take my first steps and also cautioned me that my GI tract had shutdown and this was normal so I was in liquids and salines for the day. I walked perhaps 50 steps and then back in the bed. My roommate was a guy named Phil and very nice but the absolute king of snorers. Dr EDV stopped by in the evening to see how I was doing. Of course, my wife, my mother, Susan also visited and I do appreciate their visit with me.
My night nurse was Beth and like an angel in many ways. She glided in now and then to check on me, emptied the catheter bag and so on. I should add that my urine, as drained into the catheter bag, is pink (due to internal bleeding) and I am also discarding small clots.
The hospital was very noisy at night with PA systems blasting and people chatting in the halls.
On 1/19/06, I was given numerous bags of saline throughout the day, some 10-12 in all they said. Dr EDV visited again in the evening to say I was doing well and once I am recovered from surgical effects, they would throw the kitchen sink at this cancer. Dr EDV also dispatched doctors to see me every day as well, to check on me. For example,a doctor Fiona came by today and adjusted the surgical tubes for me. My day nurse was Kathy P. My roommate Phil left today and a new man came in – he donated a kidney to his wife as she was suffering from lupus and her kidney’s failed. NoelJ was kind enough to stop by in the evening and say hello also. Later my friends Phil and John T visited; later still our friend Roseanne also stopped by.
That night I heard and felt strange noises in my body, liquids rushing through me like a hose turned on full blast. I beeped for the nurse (Michelle) and she came and pulled out her stethoscope and said my GI tract and bowels were all working – I was concerned I had a GI blockage. I weighed myself and found I weighed 10 pounds more (!).
On 1/20/06, some doctors came by and said the noises were from the 10-12 bags of saline I was given – they were essentially flushing me out. They also said I could go home today. They removed the surgical tubes and my nurse (JesseW) showed me how to empty the catheter bag by myself. His goal was to get me out by noon but he was waiting for paperwork etc. He also gave me an injection of Lupron in my buttocks as it had to go into a muscle. Anyway, Lupron tells the brain to not make sex hormones and thus not make estrogen (in women) or testosterone (in men). Without Testosterone, any remaining prostate cancer cells will die. [Of course, some of these same cells may have mutated as well].
We finally left at 2pm (me in gowns still) – KathyH met us at the curb in front and bid us farewell – she said to sit on a pillow and hold a pillow on my lap. I slept part of the way home and hobbled downstairs to the basement. They had me take Casodex for about 5 days until the Lupron kicks in – the Lupron shot is good for 3 months.
Days following
1/20/2006 KathyH recommended a product called "Scarless" which you drip on the incision 2x daily and then rub it in. It is rich in Vitamin E and other items and it does work well but it is pricey, some $45/ounce. Yet an ounce does go a long way and health insurance usually pays for it.
As I settled in at home, I immediately decided to monitor myself for a few days to insure an infection did not flare up or something else go amiss. So every few hours, I checked and wrote down my temperature (mouth thermometer), my pulse and blood pressure (a home use product that shows this) and also quantity and color of urine. My temperature fluctuated between 97.9f and 99.9 (they said to watch for 101) and my pulse stayed in a range of 68 and 100 (resting/walking respectively). Blood pressure was nominal, i.e. 105/70 at the low and 120/68 at the high. I watched myself every few hours for a few days until no real change noticed.
The pink color of the urine faded back to normal color by 1/21/2006. My family doctor called said it was a good thing I went to NYC as any hospital on the NJ side of the Hudson River would have removed my entire bladder. He also asked to be kept in the loop on my recovery. Sleeping at home was a problem as the couch on the first floor was not long enough (I am 6'4") and the recliner in the basement wasn’t flat enough. I ended up in what we call the plant room bed on my back and that sort of worked and then finally I slept on my stomach after 10 days or so had passed, with a pillow under my incision.
1/23/2006: I received the pathology report from the surgery last year and just discovered I had not posted them so here they are:


1/24/2006: My sister Ruthann was kind enough to come here as that was the first day I was home alone, i.e. with the dog etc (my sister Katie also offered but Ruthann is closer and it worked out well in the end). Ruthann stayed until Saturday morning when she and her husband Fran (he arrived Friday) went to NYC for her birthday. She introduced me to the concept of a ‘smoothie’ in which you place lots of fruit and so on – blend it up and drink it. I now mix in orange juice, pomegranate juice, frozen fruit (raspberries, strawberries, blueberries, pineapples etc), flax seed, soy powder and either milk or yogurt. It is a full meal, making 2-3 glasses of it. The goal here is to have a nice mix of fruit. Dr. EDV provided me with literature (from Cedar Sinai) that suggested a wide range of fruit, as measured by color (for lack of a better description) and dark colored fruit is apparently good to have, as is soy and pomegranate juice. I have this every day for breakfast.
Showers were something my wife had to help me initially with especially with the catheter. I simply could not bend over etc…The catheter itself was mildly irritating so I rubbed the tube where it entered my body with both Hydrocortisone Cream USP 1% and Lidocaine Hydrochloride Jelly USP 2% about every 4 hours or as needed. It definitely helped. (At this point, I cannot bend over too much and picking up a pen on the floor is out of the question).
On 1/31/2006, we went back to NYC to see Dr. EDV, with me wearing a leg mounted catheter bag. The office did the usual when we arrived, took blood, my body temperature, my pulse etc. Dr. EDV then looked at my incision and said it looks good – he removed the surgical bandages. My wife remarked that I do not feel pain and Dr EDV said I was a very good patient. KathyH then removed the Foley catheter, i.e. she drained the distilled water out of the catheter (this keeps it inflated to golf ball size in my bladder so it does not come out). Then she had me take a deep breath and said to exhale as she pulled out the catheter – essentially painless! She cautioned me about stress incontinence and said to practice the Kegel exercises often. I asked about driving and Dr. EDV said it is doable but I would be unable to stop the car in an emergency, i.e. a child runs in the street so do not drive. I asked about walking the dog and he said that was strictly forbidden.
They sent me home with CIPRO rx which is antibiotic to prevent bladder infections which can happen after a catheter is removed. I asked how long I will be out and Dr EDV said perhaps 6 weeks or less but see how I feel. I stopped off at Pathology and asked for the biopsy slides on behalf of Dr. FrankM – it costs me $20 and theoretically, they want them back someday.
Side notes: At home, I cannot bend over to pick up an item so I have a grabber which extends 30" or so and I use this to pick up a pen I may have dropped.
Also, to handle stress incontinence, I use "Serenity for Men Bladder Protection". It is a small triangular pad (48 of them for $15 at CVS) that sits in your underwear and thus any drops that come up end up on that pad. The pad is very discreet and also chemically treated to neutralize odors. I highly recommend it for those who may need it.
On 2/6/2006, my friends KevinB and JohnT surprised me with visit. They drove down from Connecticut and we went to a local pizzeria for lunch – they joked that they had bets if I needed a walker! We had a nice time and I thanked them for coming.
By 2/7/2006, at home, I am getting slowly better in that these are my only constraints as of today:
* Should not walk the dog (but I do it if no one else is home and he cannot wait but I do not let him pull me)
* Forbidden from driving a car
* Cannot bend over to put on socks or shoes.
* I still suffer from Stress Incontinence which appears to be getting better.
Otherwise, I appear to be okay but I am sure my stamina is way down. Also - my bladder now signals when it is time ‘to go’ – it did not last week. I also find getting to sleep is not as easy as it was before surgery.
Re my daily meds – I am not allowed to resume baby aspirin or vitamin E etc until one month after surgery per KathyH.
On 2/11/2006, had a tough time sleeping – coughing way too much – our 24yr old son has the Flu and maybe I have it now also.
On 2/12/2006, partially in desperation (coughing heavily less than 4 weeks after major surgery) and also with a fever of 100.7, we contacted our Family Doctor, i.e. Dr. FrankM and he called in prescriptions for me:
* Promethazine/codein syrup HIT (to stop this cough which is both bad for me and tiring).
* Zithromax, also known as Azithromycin (antibiotic) - 250mg tablets - 6 tablets
* Tamiflu (oseltamivir phosphate) 75mg gelcaps - 10 total
My fever hit 101.4 at the height of the Flu.
2/13/2006: Slept soundly from 1030pm to 830am, fever now is 99.8. Cough is minimized as long as take the syrup. My stomach area hurts today from all the coughing yet I feel otherwise okay but a bit drowsy/dizzy, no doubt from the drugs.
2/21/2006: It is 5 weeks ago today that I had that surgery and I drove my car for the first time today. I resumed my regimen of 81mg aspirin and Vitamin E supplement, per the Doctor’s okay. I am also able to pick up items on the floor – the main issues remain bladder control (Stress Incontinence) and lack of stamina. Kegel exercises are apparently essential for Street Incontinence management and I am making slow but steady progress.
3/1/2006: I met with Dr EDV today (my surgeon) and he said the incision looks great and he felt inside of me (using DRE) and said “There is no scar tissue – very good!” He also said genitals looked good also. I had occasional bleeding near top of incision and he said that was normal and he looked at it and said it is fine – just keep a band-aid on it. He said I am ready for work on 3/6 but asked I work a reduced schedule (if they let me) until my stamina comes back. He also said “You do get tired mid-afternoon and have more stress incontinence issues at that time also?” I said that was exactly right. He said see him again in 6 weeks (4/12/2006). He also said the blood they just took (they take it every visit) will be checked for PSA and it should be 0.0 and he will let me know. I asked him what is in the space where my prostate was and he said “I moved your bladder down to there”. He also suggested that when I fill my bladder full, hold off a bit before emptying it as a way to enlarge it.
KathyH also said do not wear jeans for a few more weeks yet (I tried them and it hurt to sit down). Regular business slacks and sweat pants are fine to wear.
3/2/2006: I decided to arrive at 830am at work and work until 3pm the 1st week and then the same hours the week after. I notified the VP in our office who was supportive of me. Of course this assumes my stamina supports this.
3/3/2006: KathyH emailed me to say my PSA score just came in and it is less than 0.1 - I also drove to my niece’s graduation and it was 150 miles roundtrip and I was yawning nonstop by 3pm!
3/6/2006: I returned to work today, 1st time since 1/13/2006. I arrived at 845am and left at 3pm a little tired; minor incontinence issues only. Note also today I found many fine details and pictures at this URL: http://www.urologyhealth.org/adult/
3/12/2006: after a week at work (9am to 3pm instead of 8am to 6pm), my incision flared up with two infections, one at the top and one at the bottom – in both cases, that is where they tied the sutures. I contacted KathyH and she said to use an antibacterial soap and also dap it twice a day with bacitracin (over the counter medication). I tried that but it did not help. I emailed a photo as of this past Friday to Dr. EDV asking if I need an antibiotic.

I am guessing all this activity this past week did something to me. I also had severe constipation this past week so I stopped taking Colace (!!) and KathyH said to drink my liquids and more fiber to see if that helps (surgery of 1/17/2006 was in the immediate area of my colon/rectum). She doubted Colace was the cause…I do seem better as of today. I will also try to see the family doctor tomorrow if I can and ask him to look at it. Dr EDV also said my PSA level is undetectable which is good news but then again, my PSA level was never high.
3/14/2006: I went to NYC to see KathyH and she had a doctor look at the incision and both said it looked fine and just let it dry out. I will say it looked better this morning compared to last Friday night.
3/23/2006: as a way to motivate me to hate this cancer and to show I am beating it, I posted this saying on the wall in a nice frame, centered on a tombstone backdrop
*****
Joe’s Cancerous
Prostate Gland
Prostate Born: 10/1950
Cancer Detected: 12/1/2005
Prostate excised: 1/17/2006
When I first heard the news
Not a tear crossed my eyes.
I disliked it immensely,
But then I realized
T’was my traitorous cells
That I really did hate
For turning against me
At such a late date.
So join me now in most boisterous of voice,
With A whole-hearted laugh
and YOUR verbiage most choice,
To this cancerous beast
we shall all yell
"DIE DIE NOW and see you in hell!"
[It then points straight down to a biopsy slide from my prostate which definitely has cancer cells on it. My good friend Phil contributed to the editing- thanks Phil!]

*****
3/23/2006 - Dr. EDV has me working 6 hour days for now so I do not overdo it. He advised me yesterday that I can return to a normal work schedule on 4/3 which is 1 day shy of the 11 week anniversary of the major surgery. I noticed some occasional small blood spots in my underpants overnight and I called KathyH and said this is normal and not to be concerned but let her know if it changes. Regarding constipation she said this was my body getting used to my new diet (see 1/24/2006 above) and not related to surgery. I resumed Colace (Eckerd's brand called Docusate Sodium 100mg) at this point to help and I still have my morning 'smoothie' most days and sometimes I have it for dinner instead.
3/30/06 - My wife and I drove up to Arlington VT for a friend's birthday as well as a nice get-together. It is 185 miles each way and I largely drove it. While there, I hiked up a modest mountain (perhaps 3/4 of a mile each way) with my friends and I did fine, but needed to catch my breath periodically yet so did my friends.
4/4/06 - I resumed more of a normal work schedule now, i.e. arrive at 8am and leave at 5pm. I will keep this pace for 2-4 weeks until my body adjusts to it and then go back to the regular schedule, i.e. 8am-6+pm and occasional Saturdays. I still get tired easily. Constipation is less of an issue also. MILESTONE: Today is the 11 week anniversary of that major surgery on 1/17/2006.
My sister has a son-in-law as a doctor and he recommends we have something like this (moved to 05/30/2007) every day and he says other doctors do this every day also. My NYC surgeon also drinks Pomegranate juice everyday, as do friends I know who have had medical problems - they all drink it. Hope that helps and it is not as hard as it may sound to do everyday.
Dr. EDV had previously stated that it is likely the diet that we eat that triggers prostate cancer. He stated that Asian people do not get prostate cancer at the rate we do (relatively rare) but when they move to our country and live here and eat our food, then Asians get prostate cancer at the same as every other man (although it has been said that Black people get prostate cancer at a rate perhaps 2-3x more likely than Caucasians). Also, I have read that if one gets an infection of the prostate, this may trigger prostate cancer later in life...much research is apparently underway on this stuff.
4/12/2006: I met with Dr EDV in NYC and he stated the incision looks good and no scar tissue is indicated. Regarding the top of the incision where I keep a bandaid to avoid abrasion, he said to remove the bandaid before the shower but put a new one on as needed. I asked if I should have radiation therapy (i.e. see notes after 1/9/2006) and he said probably not as my lymph glands have been removed. He then asked KathyH to give me another shot of Lupron and come back in 3 months. They also took blood to check PSA levels and so on. I noticed in my file a copy of the surgeon's report (dated 1/17/2006) and I asked for a copy which KathyH gladly gave me. I show it below (with identifying details omitted) - click on them to enlarge it so you can read all 3 pages (depending on your browser, you may then also be able to expand it much larger to easily read it).



4/14/2006: Below is a photo of the scar on 4/14/2006 and it is slowly healing (per the Doctor), compared to the photo (above) of 3/12/2006:

4/18/2006: I called to find out my PSA level from the blood test of 4/12/2006 and Dr EDV's secretary said it came back as 0.1, essentially undetectable. This is good to hear as that means prostate cells are truly dead as a result of Lupron. I am not done as he did alert me that cancer will come back in a different form sometime between 1 year and 10 years from now and we need to watch for it.
5/4/2006: I met with Dr. FrankM (our family doctor), for the first time since surgery and he looked at my incision and said it looked very good and he likes my positive attitude and said this is important as well. He took blood tests and I should hear back on PSA etc next week. They also sent me to Quest Diagnostics (next door) as I wanted my blood typed, i.e. am I A+, AB etc....I wanted this as I had always though I was A+ but the NY Blood Center said I was A- (!). The Quest test should be interesting, i.e. which one will it show?
Side Note:
Having this blog available for my record keeping, I decided to go public with it and perhaps help some other man. So I went to vistaprint.com and had this business card printed (250 for $5) (note identifying information about me removed from this image):
I hand these out to coworkers, colleagues and occasionally even to strangers. My hope is this message helps at least one person. For example, doctors say to watch the PSA score as a flag for prostate cancer but that is NOT reliable at all.
5/7/2006: I put on a pair of blue jeans (see 3/1, above) and I am able to wear them now. Back on 3/1, I could put them on but it hurt to sit down so I could not drive with them, etc. Today I was able to do that and more. So I am making slow yet steady progress. I continue to apply Scarless every day to my incision in hopes my scar will vanish someday.
5/15/2006: My PSA came back from the family doctor (tested on 5/4) and it remains 0.1 which is said to be undetectable. My surgeon said the PSA will be the marker for when this Cancer comes back, which he considers likely between 1 and 10 years from 1/17/2006. [My blood type came back as A+ from Quest diagnostics]. I still drink a mix of Pomegranate Juice and Orange Juice every day.
6/4/2006: We went to Vermont for Memorial Day weekend and I hiked 2.6 miles (in each direction) deep into the Green Mountain National forest and that was good exercise.
Also, my right ankle does hurt at times (before the hiking) and Dr EDV said not to worry and take motrin when needed...thus not cancer related in anyway. I need to ask him what else we can do besides hormonal therapy (i.e. Lupron) because literature says that is good for perhaps 1-2 years or so. Thus are there any herbs, drugs I should also consider? I continue to drink Pomegranate juice every day and those smoothies every weekend (yum-yum!).
6/11/2006: I changed my drink slightly - I now drink 8oz of Pomegranate Juice mixed with 8oz of Welchs Grape Juice. Both juices are PURE juice and the combo does taste good. You may recall that Dr EDV had said to drink Pomegranate Juice every single day. My sister also recommended ACAI berries as another possible potent juice.
6/27/2006: My nephew (a relatively new doctor) read this blog and commented, in part, as follows: "From everything I read in your blog it seems that you absolutely made all the right decisions".
7/15/2006: At a social event, I met with a colleague who also had prostate surgery and it was done at a local hospital in central NJ- the surgery was apparently poorly done, i.e. the prostate was removed but the urethra (which MUST be cut to remove the prostate) was not reconnected. This poor man has a tube instead from his bladder which takes the urine out his body to a urine collection bag and he is also said to be in constant pain and must be on pain-killers to keep the pain under control. I referred him to my surgeon in NYC in hopes my surgeon can help my colleague.
===========SIX MONTH ANNIVERSARY==============
7/17/2006: Today is the 6 month anniversary of that major surgery (see above). I met with Dr. EDV on Friday (7/14) and he looked at my incision and said it looked good- he said the top and bottom of the incision are still a bit red and that is normal.He then felt inside of me (DRE) and felt no cancer nodules or lumps and said I am doing quite well overall. They did not have a 3month dose of lupron on-hand so they gave me a shot with 4month dose. Dr. EDV asked if I am changing my diet and I said I am making good progress. I also said my stress incontinence is largely gone and constipation problems are more rare (compared to the weeks after surgery) and he said that is also good to hear. I see him again on 11/10/2006.
Below is the incision as of 7/17, i.e. six months to the day since surgery:

==================================
7/21/2006: The PSA test from the blood drawn on 7/17 came back as undetectable, which is what I hoped for!
8/25/2006: 2-3 days ago I noticed it became quite painful during normal urination, especially near the end of the urination. I contacted the surgeon's office in NYC and asked for help and his assistant (a) arranged for a urinalysis test and (b)a 7 day regimen of CIPRO which will 'cure' urinary tract infections. This was on a Friday so I was anxious to start that drug regimen that evening. The CIPRO had me starting to feel better by Sunday and by the end of week, it was gone. Interesting enough, the urinalysis came back negative, no infection. By the way, I had the same pain shortly after surgery but not as bad so I may have had a minor infection right after surgery (see 1/31/06 above). Otherwise I am doing fine but I notice my stamina has not fully returned and my wife says I still appear frail at times.
9/5/2006: we went to Vermont this w/e and my host and I went hiking and it was largely uphill and I had to stop after 1/2 mile as I simply could not do it. A few days later I notice a dull pain in my left hip joint - likely from that hike. If it does not go away in a few days, I will see a doctor to find out why.
09/10/2006: MAJOR UPDATE – Prostate cancer returns...
On the weekend of Sept 9/9-10, I went out Saturday to a nearby Greek festival and had a good time. I went to bed on 9/9 and woke up 9/10 and could NOT urinate. Instead, 6 drops of blood came out instead. I made a mental note and tried again a few hours later and 20 drops of blood and a long clot came out but again no urine. At that point I knew I had a problem. So my wife and I headed into NYC to that hospital Emergency Room. By now, I cannot sit - only stand or lay down - this is due to my bladder (30% smaller since surgery of 1/17/06) being quite full. The ER lady puts an IV port into my bloodstream and attaches it to my arm such that drugs can readily be put into my system if needed, i.e. an IV drip or whatever- this is standard procedure at this excellent hospital.
The ER people tried to put a catheter in so it would drain my bladder but could not get a catheter in me (obstruction) so they called two on-call urologists who came in and used a cytoscope (a thin tube which on the end contains a small lens and lights and a tube. From the tube comes water for irrigation). This was gently slipped into my penis and up the uretha canal and they saw the blockage and could not tell what it was. They then used thin plastic tubes to guide plastic wires up to the blockage and they (apparently) poked enough holes in the obstruction such that urine came out. They then slipped in the catheter and then used what they called bladder irrigation. Basically, they send water into my bladder and then pull it out and out comes whatever the water sweeps up. In my case the water came out pink and had clots in it. They said I was to stay the night and they would meet with their boss (my doctor) to discuss it further. So at least the urine is coming out! They (the two urologists) told me no food or drink past midnight. I promptly asked they order lidocaine for me (this greatly reduces the pain/irritation of the catheter). They took a blood test also and I asked they check my PSA level in that blood test (it came back as 0.06 - extremely low and thus generally good since I do not have a prostate that generates PSA).
9/11-Monday I wake up in room 8C242a and they immediately start a barrage of tests, i.e. EKG, two chest XRAYs, periodic bladder irrigation (about every four hours) with clots coming out every time. They also check my pulse, blood pressure and Oxygen levels 3x per day. Finally they take blood for CBC (and whatever else they check for) - this is 2x per day - very thorough. I decline all food and water as they told me last night as a procedure may be done later today. A senior doctor comes by with about 5 more junior doctors and he asks me for an update, they discuss my case and look at my surgical scar and then leave. This is fine with me as it helps the new doctors become great doctors.
Around 3pm, I mention I feel light headed and the nurse calls the doctor and he says to check my glucose level in my blood (as they would do for a diabetic) and also take my blood pressure laying down, sitting up and then standing up. They are concerned since I said I was light headed but I say this is how I get when I hungry. I then get a late dinner. I am also getting IVs now with either saline or something else - I think they are telling my kidneys to create urine so that the bladder is constantly draining. IVs all the time for me it seems.
9/12-Tuesday I get more blood tests and then a bone scan as my left hip still hurts (from the 1/2 mile hike uphill in Vermont the w/e before or is it arthritis or could prostate cancer be hitting that joint). Two hours prior to the bone scan, they put Technicium 93 (half-life is 6 hours) in my blood stream so I show up better on the scan. The technician says I would set off Geiger counters(!). After all this, they cannot rule anything out from the bone scan. That evening I am thoroughly sedated and they perform a formal cystoscopy- Dr. EDV inflates and examines the entire bladder lining with a cytoscope and take biopsies of areas that look questionable. He told me later that the obstruction was due to clots and at the 2 o'clock position, there likely is a cancerous nodule about the size of a fingernail and this is likely bleeding and sending off the clots. He ordered a biopsy but says he knows it is cancer. I go back to my room and eat and then ask for Percocet. I take this powerful pain killer until the next morning.
9/13-Wednesday I continue to get blood tests and vitals checked and am scheduled for a cat-scan (with Iodine) so no food again today(!). The first cat-scan shows the bones and then the second one is started after they put some iodine compound in my bloodstream (I develop a rash from it so they later give me benadryl via the IV) and this iodine makes the circulatory system light up so it is visible on the 2nd cat-scan. Dr. MatthewM comes by from Oncology and he and his team ask a lot of questions. Dr. EDV says I go home on Thursday if all goes well tonight. I mention to Dr. EDV that we need a better marker than PSA, i.e. another blood test to find this cancer in me and he concurs.
He orders a cytology, i.e. the cytotechnologist microscopically examines the morphologic features of the cells, relates these findings to the patient's clinical history, and renders a cytologic impression. Dr KristinH (Oncology) comes by and performs a formal physical and says I seem in great shape, i.e. no inflammations, edemas and so on. She is on rotation from Munich Germany and we discuss my case at some length.
9/14-Thursday I wake up and the catheter has a normal colored urine in it, i.e. amber/gold. So they take the catheter out and ask me to drain my bladder once and then they need a small amount to mix with some other chemical to 'fix' it. They take that away and then another set of vitals and then another blood test for CBC and so on. Finally they ask for a new blood test to see if blood chemistry is okay since I have been generating a lot of urine from the IVs etc.
I get home and all seems well until later. Urine control is fine but the color is now distinctly pink and two clots always come out and I can feel the urine 'push' the clots out. The doctor says these may be old clots but call him as needed. I am less sure....for the rest of the day, I have pink urine and clots coming out. I go to bed and sleep on my side as a hope the clots will not settle in my bladder. I wake up at 12:20am and 4am to urinate and it comes out the same, decidedly reddish/pink and more clots and this continues on Friday 9/15. I send an email to the doctor advising him of this and I am fairly certain I am going back into NYC to this hospital. Stay tuned.
Note: details on a cystoscopy: http://www.healthatoz.com/healthatoz/Atoz/ency/cystoscopy.jsp
9/15/2006: I am still passing numerous clots and my urine control is excellent but the urine color remains pink. Per Dr EDV, this is okay as long as you can pass them but if you can't, get to our hospital right away. For now, drink LOTS of water, take iron pills (Ferrous Sulfate) and stop taking Vitamin E and also the 81mg of aspirin. I also take Colace as Ferrous Sulfate is constipating and Colace offsets that. So for now, I keep drinking a lot of water and keep urinating lots of clots. What I life to live! Anyway, this coming Tuesday I meet with an Oncologist as well as Dr EDV to discuss my case and come up with a game plan for my care.
9/19/2006-I wake up today and find I cannot urinate once again (see 9/10 above). So we head towards NYC but I find my bladder is too distended to make it (traffic was terrible! It was rush hour and also the UN was in session in NYC) so we dial 911 and I take a volunteer ambulance to a nearby NJ hospital. They contact Dr. EDV and he asks they put a catheter in me and then release me. They do that in the ER and I release some 1200+ ml of urine/blood. What a relief! Next we head to NYC for two appointments. The 1st is with a preeminent oncologist and he tells me the reason my left hip hurts is because [prostate] cancer is there - it has gone through the bladder wall and attacked the Ilium area (top area) of my pelvic bone sclerotically (Sclerotic essentially reflects a thickening of the bone; lytic lesions are less common and are ones in which the bone is destroyed and replaced with tumor tissue). Click here to see a picture of the pelvic area and the iluim. They recommend chemotherapy and we are to meet with him later this week perhaps. Next I meet with Dr. EDV and he says I should come back on Friday and he will perform a trans-urethal resection on my bladder (TURB) and thus remove the small tumor in my bladder which is causing all this bleeding and thus generating all the clots. I will stay overnight so they observe me and then send me home Saturday. They send me home with a foley catheter as this should reduce the chance of a clot blocking me again. I ask them if I can perform bladder irrigation when needed and they agree I can. I go home and then my catheter is now blocked so I perform bladder irrigation and that fixed it as numerous clots came out. Bladder irrigation means you pump (previously prepared store-bought sterilized saline solution) INTO your bladder and then extract that same amount of liquid out. Doing this also clears any clot blockage I may have. I had to do this twice that evening (no doubt due to the fact I drank little water today). I have to do this nearly every day until 9/21.
Needless to say, I thought I was doing fine. Well, at least I have truly excellent doctors and a top rated hospital so I am in good hands.
9/21/2006-I wake up and my urine is finally clear! No signs of bleeding at all.
9/22/2006-Again my urine is clear! Anyway we head into NYC again. This is for the TURB previously scheduled. I know I have a clot in me that is occasionally blocking the bladder orifice and thus I need to irrigate it now and then. I tell Dr EDV there is a big clot in there and then they sedate me (using Midazolam (Versed), Fentanyl and Propofol). It goes well and using a cytoscope, Dr EDV does fulgurate (i.e cauterize with electricity) a small tumor, i.e. the blood vessels leading to the tumor site so they do not bleed (he did not remove the tumor as it goes through the bladder wall). I go home with a foley catheter the same day, with antibiotics and pain killers. I am groggy and spacey all day due to the after-effects of the anesthesia and then the percocet (pain killers). I sleep very well that night.
9/23/2006-I wake up and urine remains clear. Next step is back to see Dr EDV to remove the foley catheter and then the oncologists to begin chemo process, i.e. blood test, paperwork etc. This meeting is on 9/26; The chemo should start the week after and will likely include Taxotere and Prednisone.
9/24/2006-I wake up and urine remains clear. My left hip does hurt so I take Tylenol. This is no doubt the ilium where the prostate cancer has spread. My doctors are well aware of it so it is a matter of time before they go after it with chemo.
9/26/06-We met with Dr EDV at 130pm and he removed the catheter and we talked briefly about the prostate cancer. I asked about incontinence issues since I had a catheter for a week and they said it should not be an issue but do those Kegel Exercises to strengthen the sphincter muscle (this controls the bladder flow). I explained I also felt very powerful urges to urinate even with the catheter. Dr. EDV called it bladder spasms and said the bladder tried to expel the catheter and that is what I felt and not to worry.
He also said Lupron did kill some of the prostate cancer, based on what he observed in my bladder but if even one cell survives, then it grows and grows and so on.
Then we hurried to see the oncologist Dr. DavidN for our 2pm appointment (in the same building). His team took blood, urine samples, an EKG and otherwise looked me over. Then I agreed to a clinical drug trial. Basically, the clinical drug trial (called a protocol) is to test a new drug. As part of the protocol, I also get two other drugs, i.e. Taxotere/Docetaxel (inhibits cancer cell growth, which depends on the formation of an internal cellular skeleton made up of elements called microtubules. During the cell development cycle, microtubules first assemble and then disassemble, permitting cancer cells to divide and thus allow tumor growth. Taxotere essentially freezes the cancer cell's internal skeleton by promoting the assembly and blocking the disassembly of microtubules. This action prohibits cancer cell division, which causes cell death) and Prednisone (to offset some of the side effects of Taxotere). The newer drug is Bevacizumab (also known as Avastin) - this newer drug is FDA approved for colorectal cancer and is being tested against prostate cancer in this protocol. It has been shown (for colorectal cancer) to inhibit the growth of new blood vessels, which cancers need. Bevacizumab is a class of drugs known as monoclonal antibodies. This is a double-blind randomized test so I get at least Taxotere and Prednisone and I may get Bevacizumab or I may not. In any case, this clinical drug trial will not drive my cancer into remission but prevents the tumor from getting new blood vessel and without new blood vessels and it may well die. The issue is some of the cancer cells may become resistant to the chemo and then another approach is needed. This is all about buying time until some future medical breakthrough. Cancer these days is pretty much a disease we live with and try to keep at bay so to speak, if you can. Also, they said my daily smoothie (see 4/4 above) is perfect food for now and I am also to eat a balanced diet.
Regarding returning to work, the doctors says this is still unknown. I have an aggressive [prostate] cancer that does not respond to hormone therapy at all, the standard treatment for prostate cancer. It is also pressing up against my pelvic bone (I can actually feel it from within, like a tennis ball in me) so it impacts my walking quite a bit. Even walking around the house is not at all easy. I also have some bladder incontinence issues to work out as well.
I go to bed around 11pm and urinate and two clots come out and the urine is slightly red. This has me concerned needless to say. I go to sleep and wake up around 2am and urinate again - this time it is lightly red, no clots.
I did get some medical reports back from last week, i.e. a bone scan report and a 3 page Cat Scan report (2 different cat scans - 1 regular and 1 with IV Contrast). Below are the reports with identifying text removed (doctors, dob, etc):




09/27/2006-I wake up and urinate and it is all clear. I contact KathyH and ask for CIPRO since the catheter just came out. She calls it in to our pharmacy. Urine remains clear all day and KathyH says be sure to drink a lot of water. It remains clear all day and I then head off to bed.
There is little doubt in my mind that cancer is diet related. "Our results suggest that a high ALA [Alpha Linolenic Acid] intake is associated with an increased risk of advanced prostate cancer." Also look here. ALA is found in found in soybean and canola oils, flaxseeds, walnuts, and purslane. Of course, much more research is needed.
10/2/2006-Yesterday I noticed my inside upper left leg started to hurt...was I on the stairs too much yesterday? I took two percocet and went to bed at 10pm. I wake up today and it still hurts and I am actually concerned I cannot go up or down the stair case. Realizing Tylenol is not helping and Percocet is not either, I switched to two tablets of Vicodin Generic (5mg Vicodin/500mg tylenol) and that did work, it took the edge off nicely....Had this cancer decided to wander down my femur bone from the Ilium bone? I wonder how long before I can't walk? Chemo starts this week and I hope it destroys this strange cancer quickly. My sister thinks it is nerve being impacted by the cancer and not the femur and my contact at the NY Hospital confirmed this is likely.
At night they ordered a strange prescription drug (Dexamtheasone 4mg). It was strange in that (a) take with food or milk) and (b) take 2 tablets each 12 hours before chemo and then 2 more 3 hours before chemo and finally 2 more 1 hour before chemo. This apparently an anti-nausea drug.
10/3/2006-Chemo started today and because my Oncologist is the head of the department, I received top shelf service, no waiting, personal attention from my oncologist and his many assistants. We discussed the pain in my left leg and the Oncologist confirmed I am still strong in that leg but pain is the issue. The Oncologist stated to drink plenty of water and stay with Vicodin as needed. They took many vials of blood, i.e. 1 for CBC, 2 for unknown purposes and 4 four vials for genetic research. They also gave me a brief physical as well. Then it was time for chemo (the picture shows me getting my chemo via an IV infusion):

(Back to top)
The chemo is given in four stages (1) Prednisone (5mg) is by prescription and a tablet taken orally 2x day (with food!) (2) An IV feed into my vein with 50ml of
Kytril, it went in quickly (this is an anti-nausea drug, good for 6 hours) (3) then an IV feed of 250 ml of Taxotere over an hour (started at 2:15pm) to enter my body and then (4) an IV feed of 100 ml over 90 minutes of either a placebo or Bevacizumab (started at 340pm) but it is a double blind test of Bevacizumab so I am not told if I get the placebo or the Bevacizumab (I think it is Bevacizumab because the bag had an emulsion in it and a placebo would be 0.9% Saline instead and that would be clear). They sent me home with three prescriptions to control posible nausea and vomiting. The drugs were Zofran (5mg) to be taken 2x a day for 2 days and then as needed. Prochlorperazine (10mg) every 4-6 hrs as needed to control nausea and finally
Prochlorperazine Suppositories (25mg) 1-2x daily but that is only I am very nauseas and unable to keep food/pills down orally. In addition, they stated use Zofran for 2 days and then the others as needed. We go home and I feel fine but they said it would not be tonight but tomorrow that I feel at least fatigue and watch for other symptoms as well. Stay away from crowds (low white blood cell count may make it easier for an infection to hit me!). Stay especially away from sick people and anyone who recently had a shot. Wash hands/face often - be careful brushing your teeth as red blood cell count may also be low and thus I may bleed easily.
Let's hope this chemo hits me gently as a person and as a murderer to those nasty cancer cells. Stay tuned...
10/4/2006-My left hip (Ilium) and the top 1/3 of my femur hurts, not doubt from all that walking yesterday in NYC. Vicodin does not seem to help. Per NYC hospital, do not take more than 4 vicodims per day. My SO and my son says my face seems a little red and my voice has changed slightly. I checked myself every few hours and my blood pressure, pulse and temperature and it was all nominal and well within range. Otherwise I am doing okay. Went to bed and had trouble sleeping due to pain in my left leg. My left leg is essentially useless, i.e. I need to use my hands to lift it. It is not easy getting dressed as you can imagine.
10/5/2006-Woke up around 730am and my upper left leg is very painful. It hurts whenever there is no pressure on it, i.e. no pain when standing on it. I sat in a chair for a breakfast but had a difficult time even standing up afterwards. Took two Vicodin at 8am and then fell asleep for 90 minutes. I called NYC and they said to switch to Percocet at 2pm and stay on that round the clock - it is stronger. If that does not help, call them back and they will get me a 25mcg pain patch. No side effects yet from Chemo and my blood pressure, temperature and pulse are all nominal. Went to bed at 11pm and took one percocet.
10/6/2006-Woke up and was barely able to get out of bed or walk (left leg pain). So I very SLOWLY made my way downstairs to the Kitchen and took two percocets and about 40 minutes later, the pain was quite manageable. So as long as I take two percocets every 4-5 hours, then I am able to tolerate it. I contacted the NY Hospital and they will order me a pain patch and also more percocet. The patch lasts 72 hours and the percocet is a fall back only. They also said if my temperature hits 100.5, go to an Emergency Room; but I do monitor it and closest it came it has come was today at 100.1 and then it drifted down. Tomorrow, if local pharmacy does not have pain patch, then I will keep two percocet pills near my bed for tomorrow morning.
10/7/2006-I did wake up at 3am in pain so took two percocet then and went back to sleep and then at 8am, the pain came back so I took two more. The NY Hospital said to wind down the percocet (no more now but they did okay another prescription for it) and apply the patch of Fentanyl which delivers 25 mcg of the drug per hour through my skin. My fever has been bouncing around but once it passes 100.4, I am to call the on-call doctor for guidance. It briefly touched 101.6 and then settled down to 100.4; I did call the doctor and he said to not take tylenol as that will drive the fever down and thus mask the problem. He said to check my temp at 7pm and 11pm and it did drift down to 100.0 or so. I went to bed hoping I would not be heading to the hospital overnight. The on-call doctor said I am to ask the hospital to test me for a Neutropenic condition resulting from Taxotere this past Tuesday.
Side note: Percocet is very constipating and thus one must usually take other measures to offset these, i.e. (Metamucil, Colace, Enema)
10/8/2006-I slept through the night I woke up and temp at 8am was 99.9 and and then at 1030am, 98.9 - I will continue to monitor this all day long. My left does hurt and am having hard time walking more than a few feet...specifically, I cannot lift my left leg by itself so I cannot easily lift it to walk or to dress. I also have a persistent dry cough if I talk too much.
10/9/2006-I placed a call to the hospital oncology team re my left leg pain and they said to take percocet as well if needed. I did that and it certainly helps. Temperature today remains between 97 and 99. We go to NYC tomorrow to see the oncologists and also get a bone density test and also to give blood to see if there is a marker for this specific cancer that can show up in blood test.
10/10/2006-we went to NYC today and met with oncology team at 1pm and they took a blood sample to assess the impact on my blood cell counts. We also discussed the pain I was feeling and the Doctor recommended I get a pelvic x-ray and also an MRI of the pelvic area to see what is going on. Next we went to get a bone density scan (essentially an x-ray of the bone) and then the pelvic x-ray. We also updated our pain patch prescription and received 10 more (they last 3 days each and the 1st expired today around 11am). I applied the 2nd around 8pm tonight and I will add without a pain patch, I needed percocet and even that is not enough. Tonight I will take 2 more percocet before going to bed. Re the blood cell impacts of chemo:
| Before Chemo | 1wk after Chemo | |
| RBC count | 3.55 | 3.36 |
| WBC count | 10.4 | 3.1 (this was expected) |
| Hemoglobin | 11.5 | 10.6 |
| Platelets | 487 | 486 |
No real concerns - they do watch white blood cell count carefully. They want me back in NYC next Tuesday for blood tests and so on.
10/13/2006-Per prior arrangements we went to NYC for a 630pm to get two MRIs, i.e. one with contrast and one without it. The MRI was very confining so I asked for a break between MRI mini-sessions (each lasted 3-4 minutes). They were VERY busy and I finally had my MRI around 8pm (!)
10/17/2006-We meet with Dr EDV's team to drop off a urine sample in hopes they can find a blood/urine test for this cancer rather than I wait for it manifest itself in some other painful way. Then we met with the Oncologists and they said the Pelvic Xray and MRI did NOT show this cancer moving elsewhere (this was a concern since my left leg is not very functional and the oncologists were concerned the cancer was in my spine). They tested my left leg muscle strength and it seemed improved somewhat.
My CBC blood tests showed my blood chemistry is okay which is good news. We also picked up a CDROM with images from many of the tests I recently had (since September) and also the xrays for the bone scan. I digitize all these records as well as keep a hard copy of them all. We also picked up a prescription for more percocet as I was running low and I also told them the pain patches do not work for me. My next visit to NYC is 10/24 when I get round 2 of chemo.
10/23/2006-I am scheduled for the 2nd round of chemo tomorrow so I started taking Dexamathasone (4mg Roxa) per the scheduled dose, i.e. 2 pills each 12hrs before chemo, 3 hrs and 1 hr before chemo (6 pills in all). I also have been taking 2 Oxycodone w/ap/ap 5/325 (a generic for Percocet 5/325) every 4 hours. Note 5mg means the drug itself and 325 means 325mg of Tylenol.
10/24/2006-We arrived at the NY hospital and they took my blood (as always)and met with the oncologist team and they asked me to wind down my Oxycodone (2 pills every 4 hours) and up the Fentanyl pain patches to 75 mcg per hour. (They were concerned about the amount of Tylenol in my system from 2 Oxycodones every 4 hours). The oncologists said to watch for fluid retention and also a temperature rise. If I pass 100.5F, go to a (better) Emergency Room and tell them I likely have Nutropenic Anemia as result of chemotherapy - they will take me stat and rush antibiotics into me.
Chemo started at 2:10pm - this means they found a chair for me, hooked up the IV and then commenced with Kytril (50ml over 15minutes) to reduce the chance of nausea from the chemo which followed. Once the Kytril was done, then they added taxotere (250ml over 1hr) and this is the actual chemo drug. Finally they added either bevacizumab (or a placebo) at the rate of 100ml over 1hr. It was all over by 441pm. That night I felt a little woozy so I started my regimen of Zofran (8mg tablets) pills every 12 hours for a total of 4 pills. I still feel mildly nauseas (from the chemo) but zofran keeps it at bay nicely. I slept nicely. I noticed my GI system is a bit overactive but the NY doctors said not to worry.
10/25/2006-My urine is a little more red and I passed two small clots as I have been the last week or so. Dr EDV's team said to stop taking Vitamin E as that encourages bleeding. So I am to drink more liquids to keep the kidneys pumping water out of me. I don't feel like my normal self but I am not in any significant pain and am reasonably comfortable. The next few days will tell as chemo hit me on the weekend after chemo last time (see 10/3)
10/27/2006-Chemo has made me rather tired and my bowel movements are very loose and frequent. In addition my urine still shows bleeding (a little more each day) from inside my bladder but fortunately the clots remain small and infrequent. Dr EDV's team has me now taking iron pills, for two reasons (1) they are constipating and (2) they provide iron for the body to build up red blood cells more easily. I am mildly concerned I am getting anemic from this loss of blood and the chemo perhaps slowing down my body from building new blood cells. I have had some hair loss also. Temperature remains under control, i.e. routinely 99F or below.
Nausea from the Chemo has not been a problem for me. I did switch my pain management (per the oncologists) from 50 mcg/hr Fentanyl to 75 mcg/hr Fentanyl and that does take the edge off as I now take only one Percocet (5/325) and even then only once per every 4-6 hours. But it still hurts to walk. The pain itself has changed in that it had hurt when I lifted my left leg. Now it hurts to put pressure on it and it does not hurt as much when I lift it. I am to get a blood test on 10/31 (locally) and have that faxed into the oncologists team. Next chemo (round #3) is 11/14.
10/30/2006-I have stopped taking Vitamin E in all forms and my body temperature stays under control. Urine stills shows in the blood and Dr EDV and I spoke about him correcting that. He said he will speak to the Oncologist first and then get back to me on the next steps to take. Tomorrow I get a blood (CBC) test and have that faxed to the Oncologist by prior arrangement so they can monitor my body's response to this 2nd round of chemo. I notice my appetite is waning and I have lost some 20 pounds since chemo commenced on 10/3/2006. The pain patches (75mcg/hr, changed yesterday) do help, especially when combined with the occasional percocet.
11/1/2006-we went to NYC on 10/31/2006 to meet with the oncologist to discuss blood in urine and continuing problems with diarrhea. They also took blood tests (CBC), urine sample and said I look good overall and for diarrhea, start taking imodium but no more than 4 per day. Regarding blood in urine, it could be the cancer is dying (or growing) and a cat scan is scheduled in about 3 weeks to see. Last night I had a meatball hero for dinner and my stomach etc was VERY noisy and woke me up at 230pm for more diarrhea so today I switched to toast and food like that - bland stuff. The Oncologist called today to check on me (nice!) and I told her the blood in the urine is now cloudy, i.e. turbid and this could be cancer dying. She thought so also and said I looked better on 10/31/2006, i.e. I could walk better etc. I said I am experiencing thinning of the hair and my body temperature remains at or below 98.6 and that is a good thing. Below are some blood numbers as of 10/31/06 vs 1/9/06 (just before surgery):
| 1/9/2006 | 10/31/2006 | |
| RBC count | 4.35 | 3.60 |
| WBC count | 5.9 | 1.6 (this was expected) |
| Hemoglobin | 14.6 | 11.1 |
| Platelets | 303 | 319 |
Tomorrow I am get another blood test and also a stool sample to see what is going on in my large intestine and so on. The Urine sample came back with some minor bacteria but she did not seemed that concerned about that but said call anytime if I have questions or pain (while urinating) or rise in body temperature.
11/4/2006-By mid afternoon, I notice that I am having trouble urinating, i.e. it starts and then stops 1/2 way as though a faucet had been quickly closed. So we headed into NYC to the Emergency Room (ER) of the hospital we use. I also email my doctor re the problem and that we are heading in. We arrive at the ER around 5pm and a urologist had been dispatched to meet me there. He quickly inserts a catheter to empty the bladder which he says was quite distended. The normal bladder can hold perhaps 500cc (17 ounces) of urine but mine is 30% smaller due to the surgery of 1/17/2006 so mine is perhaps 350cc (12 ounces) in size. The doctor says mine was distended to perhaps almost 450cc (almost 15 ounces) so thus it hurt me until he was able to quickly drain it. The Doctor then irrigates my bladder, i.e. pushed sterile water into my now empty bladder and then draws it out. By doing so, he pulls out literally hundreds of small blood clots-these had caused my problem of urine control, blocking up my bladder exit. He then admits me (formally) to the hospital. They also take blood for testing (CBC, clotting factor) and I then go to bed. Note-My White Blood Cell (WBC) count is low at 1.6 and thus I am very prone to infections.
11/5/2006-They continue with blood tests (CBC, Chemistry, clotting factor). They also provide me with antibiotics (Zosyn 3.375mg in 50ml saline) around the clock to fight any infections that may develop. Again my WBC is quite low and my body cannot fight off infections by itself until my WBC gets back in a normal range (Chemo had knocked it way down). I also had a chest x-ray. The doctors also arrange I get a shot of Vitamin K (clotting control) and Neupogen (480mcg, to help rebuild my WBC). They also give me Potassium Chloride (via an IV, 20m equivalent per liter, at the rate of 100ml/hr) to boost my Potassium count. I also suffer from diarrhea so they provide me with Roperamide (2mg), as a replacement for Imodium. I still also suffer from intense bladder spasms so they give me a suppository (16.2mg belladona and 60mg of opium). My doctor also stops by and confirms they pulled out hundreds of clots from my bladder.
11/6/2006-Today I have a procedure called Cystoscopy and this involves the doctors looking inside my bladder and perhaps cauterizing any bleeding blood vessels and also getting tissue samples and so on. I am obviously under anesthesia (Versed/medazoliam) during this and wake up some hours later in a recovery area. Then I am back to my room and the doctor stops by and says the cancer is not spreading and it may well be dying based on his observation. They placed inflators on my legs which inflate about once per minute and then deflate. The purpose is the promote blood flow in my legs so a clot does not form. I keep these on until I am able to walk. They also commence a CBI (Continous Bladder Irrigation) whereby they let saline solution enter my bladder and then it comes out the catheter (it is painless). They must have put some 12-15 liters through my bladder this way. The purpose is to reduce the chance of a clot and the saline solution promotes healing of any wounds inside my bladder.
11/7/2006-A urologist came by at 620am and disconnected the CBI and said it was likely I was going home today which I do with a catheter still inside me and they also give me the okay to self-irrigate my bladder as needed if it blocks up. So I do go home on Tuesday. All is quiet the rest of the day at home.
11/8/2006-No real problems and urine remains the proper color, i.e. amber.
11/9/2006-Same comment but urine has a noticeable pink color in the morning and gets noticeably more red as the day wears on and by evening the catheter is blocking up and only with difficulty am I able to free the blockage, using self-irrigation techniques.
11/10/2006-Now I am fairly blocked up and have trouble freeing it so we head back into NYC and my doctor removes the catheter and then irrigates me again and notices no clots. He says I am to go home without a catheter and I should be okay, He says the clots and the bladder spasms were due to the retaining balloon that held the catheter inside of me, i.e. it was likely too large, causing irritation in my bladder - this resulted in bleeding and thus clots and also bladder spasms. So we went home and bladder spasms are gone (Thanks!) and the urine remains quite clear. They tell me to drink plenty of fluids (to dilute any blood which may still leak and thus reduce the chance for clots by diluting it).
11/11-12/2006-fairly normal days but my bladder is a little erratic about letting me know when it is full. Otherwise I am okay.
11/13/2006-My urine had more blood in it than it has in a week and some big clots also. I commenced drinking a lot of water and this seemed to minimize the bleeding and thus the clots. Tomorrow we go back to NYC to see the surgeon and then the oncologist for round 3 of chemo.
11/14/2006-I woke up at 6am and bladder did not work! Clogged by clots (no doubt) so we headed back into NYC. Doctor EDV inserted a catheter to drain my distended bladder and then irrigated it and pulled out clots sufficient to block me up. He said drink fluids all day and just before I go to bed, drink more and wake up overnight to urinate and then drink more water and go back to bed. If I wake up again to urinate do so and then drink more water and go back to bed. This should work fine keeping me free of clots. Then he gave me a (scheduled) 3 month Lupron shot and then we went to Chemo which first gave me an injection of Aranesp to boost my red blood cell count and then chemo started at 12:40pm - this means they found a chair for me, hooked up the IV and then commenced with Kytril (50ml over 15minutes) to reduce the chance of nausea from the chemo which followed. Once the Kytril was done, then they added taxotere (250ml over 1hr) and this is the actual chemo drug. Then we were done and came home and I took zofran to minimize naseau and then started drinking water to almost excess.
11/15/2005-I did what Dr EDV said, I drank water even as I went to sleep and then woke up as needed overnight and urinated and drink more again etc...It worked, no clots!! I will continue that today and for the next few days also.
11/17/2006-Last night I noticed some 15-20 clots came out when I urinated at 10pm; I wonder why that happened all of a sudden? Diet change? Too much activity? I go to bed and wake up at 1am and an unable to urinate - no doubt a clot is blocking the bladder exit and thus only a few drops of blood come out. We head to a local Emergency Room and they put a catheter in me to drain the bladder. Out comes some 1000ml of fluid (so they say)...is that possible there was that much fluid in my bladder?? The fluid coming looks to be urine with a pink tinge to it and 2-3 clots also come out. The ER doctor says leave the catheter in and contact my urologist in the morning which I do and my doctor says leave catheter in all w/e and likely see him on Tuesday. I wake up today and catheter bag shows largely urine (with a faint pink tinge) thus far and I am continuing to drink a lot of water (to keep blood diluted and thus harder to clot and also to ease the exit of clots that do form and float in my bladder.
11/18/2006-I woke up today and felt nauseas so my SO suggested I try Perclhorperazine as an alternative to Zofran. After a few hours, it was clear the Perchhorperazine was NOT working (for me) so I took my Zofran and that worked great. My bladder output was urine colored all day but then that evening, I went to bed (walking up 2 flights of stairs from the basement) and then moved some extension cords and rearranged my pillow and then I quickly notice the bladder is now putting out a much redder color of urine. Clearly, a clot had broken loose in my bladder (see below*), I went to bed, drinking water to hopefully dilute the blood such that it will not clot so readily.
*My surgeon said earlier that the cancer in my bladder was not growing and may in fact be dying. If so, the blood vessels feeding it may no longer have cancer to supply and thus more easily bleed. There is a cat scan scheduled on 11/28 to confirm this.
11/19/2006-My catheter exit hose (from the bladder) showed dried blood in it and the collection bag was not that full - so am I blocked again due to clots? I walk downstairs to the basement, resigning myself that I will have to irrigate it (flush water into my bladder via the catheter hose and then remove it) but by the time I make it to the basement, all the fluid had come out, including some clots. About an hour later, the catheter ceases emptying so this time I do irrigate myself and I pull out 20+ clots. I also had a minor bladder spasm which forced fluid out around the catheter hose instead of through it. The day itself is uneventful otherwise.
11/20/2006-Slept well overnight and only urine came out while sleeping. I continue to have stomach aches, little desire to eat and remain nauseas. I had a bowel movement and the color coming out the bladder immediately became more red (UGH!). By 6pm, no fluid coming out of bladder so I irrigated myself again but could not push the saline fluid INTO my bladder - so the catheter hose itself is blocked with clots. I pushed harder and that pushed the clots back in and then I pulled more out. I think one clot is still in my bladder so I am resigning to drinking a lot of fluids and then hoping that this will dilute the clot, making it easier to take out later if needed. Note: I will be seeing my doctor soon to discuss this and see what he wants to do. Tentatively scheduled for 11/21/2006. In the evening, I took another zofran as I felt nauseas - the good news this (expensive) pill is good for 12 hours.
NOTE: Each time I have chemo, it impacts me differently. The first time was a dangerously high body temperature. The second time was my GastroIntestinal tract was impacted, i.e. diarrhea etc. This time, it is a stomach ache and a feeling of naseaus and general malaise. I also note that I no longer need to take percocet for pain and my left leg is starting to respond better - perhaps the cancer is really being hit hard by the chemo.
**NEW 1/9/2007**
11/24/2006-I was doing fine until 11/24, the day after Thanksgiving. I woke up on that Friday and noticed what came out of Foley catheter appeared to be largely blood. This continued throughout the day.
11/25/2006-Again, I woke up and more blood - I am now concerned I am losing too much blood (via my bladder which likely has broken blood vessels from the cancer) and these ruptured due to moving around. Am I losing blood beyond my body’s ability to replace it?? I call the NY Hospital and they ask if I feel lightheaded or dizzy and at that moment I do so they said come in right away via the ER. We drive to NYC, go to the ER and they quickly notice my blood pressure varies as I stand vs. when I sit. They admit me and the Urology team then pulls out numerous clots from my bladder via irrigating it via the Foley (they push saline water into the bladder and then pull it out the same way, with the clots. Sometimes clots are quite large and it takes multiple attempts to break them up and then extract them). Irrigating is not painful per se but distending the bladder with saline and then shrinking it again when you pull water out is uncomfortable. Below is a picture of me in the hospital emergency room once they decided to admit me:

Back to top
11/27/2006-(Monday). I am admitted Saturday (11/25/2006) night (and discharged 12/7/06) and it is a quiet day all around. I am not sure of the next steps. My urologist (my primary care doctor and a senior doctor at this hospital) stopped by last night in the evening and says he will do a Cyctoscopy today in hopes of stopping the bleeding and seeing what is happening in my bladder. (I should add that I did receive a total of 6 units of blood via transfusions while I am in the hospital - 4 units right away and 2 more near the end of my stay. An adult male like me normally had 8-10 pints of blood in them and a unit of blood is about a pint of blood. Clearly, I was dangerously anemic with some 50% or more of my blood missing!)
My doctor does the Cyctoscopy (knocks me out, inserts a flexible camera and related tools into the bladder) and told me he had never seen so many clots (which he largely removed). He also fulgurated the bleeding blood vessels in my bladder (cauterized them so they stop bleeding, for now). I also have a bone scan today, to see if cancer has spread elsewhere.
11/29/2006-They have me on 'Continuous Bladder Irrigation' (CBI) now to reduce the chance of more clots. A CBI means they drip saline into my bladder via the Foley and then let it drip out via another hose within the Foley. They likely pushed through about 500 ml (a pint?) every hour or so. They also take me for a cat-scan and also for chest x-rays. The chest x-ray is likely to see if I have a tendency towards pneumonia (due to inactivity of laying in bed) and the cat scan is to get a better look at my pelvic area to see where the cancer is now.
My primary care doctor stopped by and said cancer is still confined to left pelvic area (Ilium bone) and I may need to use a walker to keep the load off the left pelvic bone where the cancer is invading. He also said the rest of my body looks fine.
My Oncologist stopped by and said Taxotere is NOT working (despite being the gold standard) so he wants me to switch quickly to new drugs (Etoposide and Cisplatin). He also said my prostate cancer is now more like 'small cell anaplastic cancer' and will be treated accordingly with these new drugs. He is cautiously optimistic these drugs will have a better effect.
11/30/2006-Today was a little difficult medically, i.e. I was getting bladder spasms-these are when my bladder senses a problem and literally FORCES itself to empty via my urethra, almost explosively. This can happen if the bladder gets too full or I feel a bowel movement or flatulence coming. Anyway, I usually hop out of bed when I feel a bladder spasm coming - this way the bed does not get messy and it ends on the floor instead. The pressure it comes out is truly amazing in that it can force the saline in the CBI hoses to go the wrong way, back up to the bags!. Fortunately, these spasms do not hurt per se but it is a very powerful sensation indeed. If my bladder is blocked due to clots, this can force a bladder spasm also. In that case, I need to self-irrigate and get these clots out. Our bladder is largely a muscular bag so it is a powerful muscle indeed. Today I likely had 5 bladder spasms for a variety of different reasons. Note-the bladder holds about 500-600ml or something between 1 pint and 1 quart (1000ml). We feel the urge to urinate around 300ml or about a ½ pint of urine which is collected via the Ureter tubes from our Kidneys.
An oncologist assistant stopped by and provided more details on the new chemo drugs, i.e. I get it at a 1/3 level each day for 3 days.
My primary care doctor stopped by and stated I may need physical therapy for my weakened left pelvic bone and need to use a walker. He also said that they may move kidney output to external bags and not to the bladder to give my bladder a much-needed rest.
NOTE: I continue on the CBI all day and night, i.e. large quantities of saline being dripped into my bladder via one tube and exiting via another tube, all to keep clots from forming, simply by diluting the blood.
12/1/2006-I get a pelvic x-ray today and I noticed my bladder hurt a bit so the nurse slowed down the CBI rate - it was causing turbulence issues inside my bladder. Around 12noon, the new chemo started, i.e. first I get Kytrile (to prevent nausea) via my IV. Then I get Cisplatin and then 1000 ml of saline and then Etoposide. Cisplatin can damage the kidneys and that is why they add 1000ml of saline right after Cisplatin, i.e. to get the kidneys actively working and keep them working. I also had a number of bladder spasms today and pulled out (via self-irrigation) some 40-50 clots.
12/2/2006-Round 2 of chemo is today. Had more bladder spasms also, including at 11pm when both outflow bags from bladder became full and my bladder could not release more urine so another bladder spasm forced bladder to exit and bypassing the tubes/hoses completely.
Side note, the staff takes blood tests at least 2x per day just to closely monitor me and I continue to have the IV (Intravenous) connection for allowing drugs to get into my bloodstream directly.
12/3/2006-Urology team put me on 'complete bed rest' out of concern for my weakened left hip. I can sit in a chair but need a walker to get there. A physical therapist came by to show me how to use a cane and a walker. That night I was given an injection to boost my white blood cell count. This is because chemo can impact the body's ability to make red/white blood cells for a period of time.
12/4/2006-A few bladder spasms today and they also scheduled a 'Percutaneous Nephrosutomy' for tomorrow, i.e. take output from kidneys to an external bag instead of my bladder, effectively bypassing the Ureter tubes which take urine from the kidneys down to the bladder. The Ureters do not work by gravity – they are muscular and push the urine down to the bladder.
Side note: I am getting Zofran as needed for nausea. Kytrile does the same thing but is good for 12-24 hours only. Zofran is also good for 12 hours.
12/5/2006-An orthopedic doctor stopped in at 6am and looked at how my left leg movement is. He then said I can use my left leg fine...I asked why I was told 'complete bed rest' was mentioned and he said that was precautionary at the time but now they know it is okay. He did say if pain increases, let them know.
At 10am, I was taken to the Interventional Radiology Department for the 'Percutaneous Nephrosutomy' procedure. They knocked me out with Versed and then cut into and through my back muscle wall to reach the kidneys and placed collecting tubes at the base of the collecting ducts of the kidneys-the two incisions are small(perhaps the diameter of a small pencil). I woke up at 2pm or so, very groggy and went on pain killers right away.
12/6/2006-This is a GREAT hospital, ranked as the best in the tri-state area and #6 in the nation. It is NY Presbyterian Hospital on 68st. and York Ave (near the 59th street bridge) in Manhattan, closely affiliated with Cornell & Columbia Universities. The Urology team is ranked #3 in the nation.
Today they brought a dog in to visit with patients so I met a nice black Labrador Retriever ('Simon') dog. They also hand-deliver crossword puzzles, books, magazines and you can have the newspaper delivered to your bed! This is why we have been coming here all this time - excellent doctors, nurses, staff etc. One senior doctor told me 5,000 doctors apply for a job there every year and they only hire the 100 best (a 98% rejection rate). So where do the 4,900 doctors end up? You get the idea....
I continue to get injections of Neupogen (480mcg) for a total of 6 days to boost my WBC. Tonight I also get an injection of Darbepuetin (100 mcg).
12/7/2006-I went back to Interventional Radiology Department to insure the procedure for 12/5 was in good shape (it was). They simply checked it using a complex x-ray system. I received another injection of Neupogen. They finally discharge me at 5pm, (after 13 long days). It was a tough car ride home, what with hoses (to my kidneys) in my back and a Foley hanging on my leg.
We arrived home and I went to bed at 9pm. I have three tubes in me(!) - the Foley catheter and two Kidney bags. The Foley catheter had blood in it when I woke up. I also notice dried blood around my urethra. My sister ('Joan') is here from Colorado and she is a RN and a Nurse Practitioner. She is a LIFE SAVER for me more than once, i.e. she can readily give me shots etc. Sadly, I have hemorrhoids and Joan says use witch hazel to ease discomfort and help shrink them. She is 100% correct. I go to bed approximately 9pm for the night
12/8/2006-I sleep well, getting up at 9am. I stand up and the Foley (leg) bag fills with apparently blood and has some clots in it also. I also notice small blood stains in front of my underwear. My sister Joan says to switch to ferrous fumerate instead of ferrous sulphate as the later is constipating. She finds ferrous fumerate in a prenatal multivitamin at CVS so I commence taking that multivitamin. At home I also scheduled to get two more injections (one per day) of neupogen while at home, given as always in a subcutaneous manner (in a muscle or just below the skins surface).
Later in the day, I develop a dull ache in my bladder and then an intense bladder spasm discharged a lot of blood - quite a mess. Pending flatulence was likely the cause of this spasm.
I went to bed around 9pm. I woke up briefly around 11pm and thought I was back in the hospital when I saw my wife come in the room. She said you are home and safe and sound and that relaxed me immensely. I keep applying preparation H (or witch hazel) to my hemorrhoids and they are slowly shrinking,
12/9/2006-I wake up and catheter bag and kidney bags are the proper color, i.e. urine colored. I head downstairs to the kitchen and feel another bladder spasm coming so I stand up (from sitting) and out comes more fluid and some clots. I self-irrigate myself and pull out many more clots, some quite large. The trigger of this spasm was pending flatulence.
I notice I cannot sit in a recliner with the kidney bags as they work by gravity and the high arms on the recliner mean the bags are too high.
Side Note: I am taking zofran for nausea and also use xylocaine gel on my urethra to keep the discomfort level down while using a Foley catheter. Zofran is VERY pricey-it retails for about $50 per pill so a prescription of 10 pills is $500! I went to sleep around 830pm and was asleep quickly.
12/10/2006-I wake up and Foley bag is decidedly urine color with a pink tinge, a nice improvement. No other news worth mentioning for today.
12/11/2006-No news except yesterday was the last day I had signs of bleeding in my bladder. What an experience it has been since September dealing with bleeding in my bladder, bladder irrigation, bladder spasms, etc.
12/12/2006-We went to NYC to see the medical people and they said they went the Foley out soon. He also said I am not to take Vitamin E or Baby Aspirin (thins blood and thus promotes bleeding and inhibiting clots). I asked re changing from Ferrous Sulphate to Ferrous Fumarate as the former is constipating. My blood test shows my RB counts are low so they gave me a shot of Aranesp (500mcg) in the usual subcutaneous manner
12/13/2006-no real news except I finally feel hungry.
12/14/2006-woke up and measured volumes of urine in the three bags, i.e. the Foley bag had about 500 ml, the left kidney bag had 650ml and the right bag had only 225ml of urine. I also gently irrigated myself and let the bladder contents drip out (again gently) - all this is preliminary to taking out the catheter. In the afternoon, my sister Joan (a registered nurse) removed the catheter and I then commenced Kegel exercises to reduce bladder leakage since those bladder control muscles were weakened due to the catheter's presence --- I have had a Foley catheter from 11/17 to 12/14 (replaced on 11/29) and that is a LONG time, the longest I ever had a catheter in me.
At home, a nurse comes by every 2-3 days to change my dressings on the two kidney connections. My sister says never get dehydrated as this drives up your pulse rate, raises body temperature and drops blood pressure....the message is drink plenty of liquids, i.e. the equivalent of 8-10 glasses of water per day.
My neighbor is a physical therapist and he dropped off weights and stretching equipment and showed me how to use them. He also endorsed shark cold water liver extract with squalamine as sharks do not get cancer. My primary care doctor however said no to exercises.
Side note: due to pain, I am now taking 2 percocets every 4 hours and also 75mcg/hr of fentanyl via a skin patch. By mid January, this has dramatically changed and the pain is largely gone. The pain was in my left pelvic area where the cancer was pressing against my pelvic frame.
12/15/2006-no real news except I am drinking a lot of fluids.
12/16/2006-woke up at 2am due to loud noises in my lower abdomen and then I noticed an intense pain in my right flank area, as though I was stabbed with a knife. The pain is intense and knocks me down to my knees. Only percocet every 3 hours keeps it semi-tolerable. We call the hospital and they recommend I come in right away via the ER. We arrive at 715am and they check vitals, draw blood, etc. The Intervention Radiology team checks me via their complex x-ray equipment and state they see my left Ureter blocked but that is not the cause of the pain and they say "your pain is not from our work". I thanked them and later had a cat-scan. I also have x-rays and numerous blood tests and they also took urine samples as well. We finally left the ER around 11pm after urology states all looks fine and ask I switch to motrin and percocet instead of just percocet. The downside of this day is I have not eaten all day as food interferes with many tests so I am very hungry. I ate something and then headed home and slept until 1pm the next day(!). The pain went away after 2-3 days and is likely due to a muscle spasm.
12/18/2006-Dr DavidN (oncologist) called as he had looked at the cat-scan from 12/16 and said Merry Christmas to me and my cancer has shrunk more than 20% in volume from the new chemo!!!....THIS IS THE BEST CHRISTMAS PRESENT EVER!!!!!!
12/19/2006-12/25/2006-Each day is about the same, i.e. still on antibiotics (levaquin) and pain killers (Fentanyl) and taking it easy.
12/26/2006-Back to NYC for day 1 (of 3) of 2nd round of Chemo, i.e etoposide and cisplatin. Arrived home in the evening and felt acid reflux coming, nausea and so on. Took Zofran to offset nausea and otherwise took it very easy. This chemo is strong stuff.
12/27/2006-Day 2 of chemo and more of the same, i.e. nausea, very fatigued and so on. It just wipes you out.
12/28/2006-Day 3 of chemo and the last day....more of the same. Good news is I am in less pain so now I am down to 50mcg Fentanyl (from 75mcg).
12/31/2006-Got sick from the effects of the chemo.....had been feeling nauseas since chemo and I need to take medicine aggressively to keep nausea under control.
1/1/2007-Still managing feeling of nausea from the chemo of last week, zofran and other drugs do keep it under control.
1/2/2007-Back to NYC to see oncologist and get blood work to see if my RBC and WBC#s are okay. He said only 4 rounds of this chemo also (it is too toxic after 4 rounds). He asked me to collect 24 hours of urine to see how my kidneys are holding up - the chemo drug cisplatin is tough on the kidneys.
1/3/2007-Felt much better today and decided to try 25mcg of Fentanyl.
1/4/2007-Completed 24 hours of urine collection (1900ml) and submitted with a blood test (required) to Quest in Wayne, NJ with instructions to send analysis to my oncologist via fax.
1/5/2007-1/9/2007-no major news
1/10/2007-Went to NYC for a cat-scan and bone scan....for the cat-scan, I had to drink 1000ml of a water solution that also contained some iodine. The purpose of the iodine is to block x-rays such that my GI tract will show up on the x-ray. For the bone-scan, I get an injection of Technetium 99M as this diffuses throughout the body and highlights the bones. Technetium 99M is radioactive with a half-life of 6 hours. The hospital generates this onsite from radioactive Molybendum. Click here for more details on this process.
1/11/2007-No major news
1/12/2007-My surgeon's assistant called and said the cat-scan report said all looks good and the cancer is not growing. I asked her to also consult with my oncologist whose call I am also waiting for.
1/15/2007-The oncologist did not call but I am back in his office tomorrow for round 3 of chemo. (Each round is 3 days in duration). I should see him tomorrow. This chemo is strong stuff and usually knocks me for a loop for about a week after, fatigue, nausea, etc.
1/16/2007-We resumed chemo, round 3 (of 4), day 1 (of 3) and the drugs again are etoposide and cisplatin - strong stuff....we did see the oncologist and also received our copies of the radiologist reports for the bone scan and ca- scan from 1/10/2007. The oncologist said the cancer shrank some more but not as dramatically and we asked re calcifying as shown on the cat scan and he was unsure what that meant and we may need a biopsy to be sure. He did show us the cat scan from 1/10/2007 side by side with the one from 12/16/2006 and the one from 1/10/2007 was noticeably brighter from the calcification. The cat scan also stated the cancer
is shrinking in some spots also but not others but it is not growing.
I contacted my surgeon (DR EDV) and he stated that “Calcium in a tumor under treatment usually means necrosis or cell death so I take it as a good sign”. I am waiting to hear from two other (unaffiliated) doctors also (one in San Diego and the other near San Francisco) to get their opinion on 'calcifying'. That evening, the chemo triggered some acid reflux so when I went to bed I used pillows to keep my chest area/had higher than my stomach so the acid from my stomach would not reflux up to my esophagus and damage it. The reflux only lasted one day.
1/17/2007-This is day 2 of 3 of chemo and also the 1 year anniversary of the Radical Retropubic Prostectomy when Dr EDV removed the cancerous prostate, some 19 lymph glands and 30% of my bladder, all of which showed cancer.
1/18/2007-This is the last day of this round of chemo and surprising I feel okay but I know it usually hits me for a few days after chemo ends so I am on guard so to speak. I slept quite well in fact which I really need. The tubes to the collecting ducts in my kidneys are still there (see 12/5/2006), but next week they will put dye in the tubes to insure my ureter tubes (which connect the kidneys to the bladder) are not blocked and then the week after, they may remove the tubes they put in on 12/5/2006.
1/19/2007-At home, a nurse came by (scheduled visit) and supervised my SO giving a shot of neulasta (boosts the white blood cell count).
1/20/2007-Chemo hit me hard today - by 130pm, I had to lay down to keep nausea under control as well as deal with fatigue. My intestines were making all sorts of gurgling noises so I switched to crackers, soup and toast to keep things quiet. I continue to take Zofran every 12 hours to keep nausea down and it does work.
1/21/2007-This is the weekend after chemo, when it usually hits me and today is no different, I laid down at 2pm and by 530pm, I thought I had died and then revived...I eat crackers and toast only for now and take zofran religiously every 12 hours to keep nausea under control. What a life!!
1/22/2007-I feel somewhat better....the chemo does kill the bacteria in my GI tract and thus I need to eat bland stuff until the bacteria comes back. Still on Zofran as I feel nauseas.
Side note-My two kidney bags are not evenly full each day and thus the kidneys are still feeding my bladder to some degree. The good news here is that my ureters are apparently not blocked. (The ureters are muscular tubes which take fluid from the kidneys to the bladder).
1/23/2007-We went to NYC today to get a blood test and meet the oncologist. He said the next chemo is the last for this drug, at least for now. After this last chemo (#4), he will schedule a petscan and a catscan. The petscan will track the metabolic rate of the tumor. He confirmed that calcification of the tumor (see last catscan report) is likely good news. We asked re the results of the Quest test whereby I collected urine for 24 hours. He said the urine function test was good. He also said it would be wise to get a hearing test as a precaution so we need to schedule that. On the way home in the car, I started feeling lousy, i.e. the vibration of the road was upsetting my stomach so when we arrived home, I quickly laid down and that helped considerably. I had light food for dinner, i.e. toast, crackers, soup. I feel asleep around 11pm
1/24/2007-I am still constipated so my sister (who is an RN), suggested prunes and a lot of water to ease it. Otherwise, today is uneventful and I feel better and ate quite well.
1/25/2007-nothing unusual
1/26/2007-I did not take zofran yesterday but needed it today in the evening.
1/27-29/2007-I have stopped taking zofran and the only event worth noting is I am now able to sleep on my stomach (my normal way of sleeping) but I do wake up (briefly) in the middle of the night and then go back to sleep until usually 8am or so. It is likely I am half-awake and being mindful of those kidney tubes, the attached bags and so on. They cannot be ignored while sleeping, especially if you move around when you sleep, which I sometimes do.
Tomorrow I am back in NYC and they will put dye in the kidney tubes to see if the ureters are not blocked and I am told the tubes may come out also.
1/30/2007-what a day! We did go to NYP and the Interventional Radiology (IR) team injected dye into each kidney, slightly distending it. I felt mild pain deep inside of me when they did this. They then said both ureters are clear and working fine (the IR team on 12/16 felt the left ureter was blocked). This IR team said both ureters are working fine and gave me the choice:
1-Leave kidney tubes/bags in place (not recommended, no need to do it)
2-Remove kidney tubes/bags - the downside is if my bladder acts up (clogs as has happened so often last fall), they would, on an emergency basis, have to insert new tubes in me, i.e. surgery (see 12/5/2006).
3-Leave tubes inside of me (capped) but remove bags. Thus if bladder acts up, we just unplug the tubes and hang new bags, i.e. no new surgery.
I opted for choice 3 and then we went home.
That evening my (body) temperature started drifting up (100.2, 100.4, 100.6 upto 101.0). We placed a call to the NYP Oncology team and NYP IR team. The oncology team called back and said to go to a local ER and state I am likely NeutroPenic. We went a nearby ER and they did two chest XRAYS and also a urine test and some 6 blood tests (of various types). They eventually said it was a Urinary Tract Infection so they quickly put me in Zosyn and then Vacomycin and also wrote an Rx script for levaquin. We ended up getting home around 430am(!).
2/1/07: Since the summer of 2006, I have lost some 30 pounds(!). So I get cold easy in the winter. The weight loss is likely due to inactivity as well as loss of appetite as a result of numerous rounds of chemo (some 7 rounds thus far).
2/2/2007-I think I have caught up on my sleeping requirements now....I still have a dull pain in my left flank area, much like 12/16/2006 but not as severe. My bladder is working fine, i.e. signaling me when it is full and I urinate fine and no sign of blood, in stark contrast to the fall of 2006 when it was routinely blocked by blood clots, as a result of bleeding within my bladder-this internal bleeding in my bladder resulted in numerous hospitalizations last fall.
I am eating fine as well and I am getting ready for 4th round of this chemo next week, i.e. stocking up zofran etc. I resumed my multivitamins and lopid and I do take levaquin in the midafternoon as I must not take it within 2 hours of the multvitamins (which contain iron).
2/3/2007-Developed a minor pain in my abdomen...could be something I ate or not so I will need to watch it.
2/4/2007-Pain is greatly reduced in my abdomen so it was likely something I did eat. The local ER where I was some days ago (1/30/07) called and said urine culture was positive and Levoquin is the proper drug to treat it so stay on it for the full regimen.
2/6-8/2007-I am back in NYC for the fourth and likely final round of chemo. Each round is 3 days long (the drugs are too toxic to have all in one day...the drugs continue to be 500 ml Saline (to activate my kidneys), kytrile (to keep nausea down), Etoposide, Cisplatin (both are potent chemo drugs) and then 500 ml Saline to keep kidneys busy as cisplatin is dangerous to idle kidneys). While there I also get a shot of Lupron (this drug helps kill prostate cancer cells in a different way and the shot is good for 3 months). I take zofran (anti nausea) each night to fight nausea feelings. I will likely be on zofran for about a week. At night the chemo tends to cause acid reflux (GERT). I mention this to the doctor and she prescribes ranitidine (150mg) and says to ignore the Rx label and just take one pill at bedtime. I also asked her re when can I drive again and she said not now and perhaps for a while (left leg weakness and also my fentanyl patch which is strong narcotic; dosage is 25mcg/hr).
The Oncologist's assistant stopped by and said get a blood test next Tuesday at 1030am BEFORE the IR tubes are removed at 1pm that same day from my kidneys (to insure my white blood cell counts are high enough.) My urologist also said to start levoquin this coming Monday as a precaution. The Oncologist's assistant also said I am scheduled for a Cat-Scan of my chest, abdomen and pelvis at 1130am on 2/21/07 and then a combined Pet-Scan/Cat-Scan at 130pm.
2/9/2007-My sister (an RN) administered a previously scheduled injection of neulasta, to help boost my white blood count).
2/11/2007-I am still quite dependent on Zofran to keep nausea under control. The chemo started hitting me on 2/9 (a day early) but not quite as bad as last time and over 3 days, not two. But I know I will be very dependent on Zofran and bed rest for much of the week. In terms of eating, I am eating small bland meals also, again to keep nausea feelings down. Zofran in fact is not enough (one pill every 12 hours) so the oncologist said take the pill every 8 hours as well as another anti-nausea drug. This seems to help.
2/12/2007-Uneventful except I am battling nausea all day. I am also waking up at 3am or so to urinate - not sure why but I urinate and then off to bed again. I am back in NYC tomorrow to see the oncologist and also get my kidney tubes out.
2/13/2007-The oncologist runs a quick blood test and says my White Blood Cell count (WBC) is okay so he okayed getting the tubes out. He does spot my RBC counts are low and orders a shot of Aranesp. This one shot costs $5000 (ouch!) but it rapidly boosts the RBC counts. Having a low RBC means you are routinely tired while a low WBC means you cannot battle infections.
Anyway, I go to the IR team and they have me get into surgical gowns (this is routine). I then lay on a table in their OR and they inject a small amount of dye into each kidney to insure the ureters are not blocked. The dye dilates the kidney somewhat and thus the kidney forces the dye into the ureter rather quickly. The OR team is watching on some digital real-time xray so they quickly see my ureters are working fine. Each kidney, when dilated, does hurt slightly in a funny way, i.e. a dull pain deep inside of me. The OR team now takes the tubes out and I then sit up and notice the right side hurts more than the left. They said this is normal and take pain killers as needed and it should clear up in 3-4 days. I ask re internal urine leakage and they stated the kidneys will close the hole quickly (1-2 hours) and the overall hole will close up in a few days. I ask re pain killers and they do not have any. [We asked a friend in the hospital and she quickly gave me two percocet capsules 5mg]. That evening my fever rises somewhat (recall Dr Vaughan has me on Levaquin, a potent antibiotic) so my sister (who is an RN+) said to drink water as dehydration will raise the body temperature and raise the pulse as steps to offset lower blood pressure. I drink a few cups of water and my temperature drifts down from 100.5 to 98.4 over the next few hours. I have a fitful sleep due to pain.
2/14/2007-I call Dr Vaughan's office and KHart prescribed a muscle relaxer for my back; between that and the use of a heating pad and pain killers, the pain is not as bad after a few hours.
2/15/2007-I feel about the same and coughing does hurt (in my back). I continue with pain killers and muscle relaxers and zofran all day.
2/16/2007-I wake up and the pain is bad - my sister said it is time to manage the pain and not just chase the pain, so to speak. She says take 3 percocets: 1 every 30 minutes for 90 minutes. This works and then I fall back to a less aggressive schedule of pain killers. Joan thinks the pain is triggering muscle spasms so we continue with pain killers and muscle relaxers and the heating pad. Later that evening, I did get sick and not sure why. Since I had already taken zofran, I then took compro as they both battle nausea but in different ways. I went to sleep
2/17/2007-work up at 6am to urinate and then fell back asleep. The day is like 2/15 and 2/16 otherwise but I did not get sick.
2/18/2007-woke up at 140am to urinate and then fell back asleep. The day is uneventful, i.e. like the last few days, with zofran, pain killers, muscle relaxers and heating pad. But that night I took a pain killer and zofran on an empty stomach and promptly got sick again. My sister said to always eat some crackers or milk before taking pills as pills alone secrete chemicals into the stomach and the stomach does not expect them alone and signals to the brain which triggers the vomit reflex.
2/19/2007-Today I slept the entire night and feel better and thus is eventful. I still take pain killers but I stopped zofran for now
2/20/2007-slept through the night again but woke up with back pain so I quickly took an oxycodone (percocet plus 325 mg of tylenol) and that helped. The day is otherwise uneventful and I feel much better.
2/21/2007-Today we went back to NYC for two tests, a Catscan and then a combined Catscan/Petscan. The total time is about 6 hours,mainly due to bad scheduling and lots of waiting time. Here are the details on each:
CATSCAN (Computer-Aided-Tomography)PROCEDURE:
For a catscan (in my case), first they ask to you to drink a liter (about a quart) of a water-based liquid which tastes mildly bitter and has a slightly brown coloration to it. After you drink this liquid, one needs to wait about 90 minutes so that it makes its way through your body. The liquid has a small dose of iodine in it and the purpose is to coat your insides with a small amount of iodine, i.e. the catscan will readily detect the iodine and thus it 'lights' up your stomach, intestines and so on. This makes it easier for the medical people to review the catscan images. Just before the catscan, you drink a small glass of a bubbly liquid - this liquid reacts with your stomach acid and (mildly) inflates your stomach (for easier viewing). During the catscan, you lay on a table with your feet facing the catscan machine. They turn it on and make sure it is working; then the table moves toward the catscan and the catscan machine says "breath deeply and hold your breatth". Then it moves you slowly into the catscan machine as the x-ray machine spins about once per second. You hold your breath about 10 seconds or so as the machine takes x-ray slices of your body-your arms are extended above your head. The whole process takes about 10 minutes and is quite simple and painless. I should add that you can have no metal (belts, watch, jewelry) on you so in my case (and everybody's case), they ask you to remove your clothes and put on a hospital gown for this (and many other) procedures.
PETSCAN (Positron-Emisssion-Tomography) PROCEDURE:
For this test, the detection process is different. To start, they inject you with a small dose (10ml) of radioactive fludeoxyglucose (Fluorine 18)which can be used as tumor marker namely, increased glucose metabolism by many cancers. The F18, being radioactive, has a half life of 110 minutes, i.e. the radioactivity decreases by 1/2 every 110 minutes. Being radioactive, it emits both a neutron (an atomic particle) and a positron (anti-matter version of an electron). The positron then hits an electron and the two annihilate (disappear) in a minute flash, also known as scintillation. The scintillation counters see the gamma rays given off and thus the PETSCAN equipment detects these gamma rays and where they occur. My sense is the fluorine atom decays down to oxygen as a result of giving up an electron but I have not confirmed this.
Anyway, for a PETSCAN, you first get that injection and then they ask you to lay down for an hour, i.e. sleep or just listen to music. The point is you are not to move and the lack of movement also gives the fludeoxyglucose molecule time to spread evenly through your body. If you move, then this same sugar-based molecule goes where it is needed (for muscle movement as an example). Instead, if you lay still, it will tend to head to areas of higher metabolic activity, i.e. cancer.
As far as getting the Petscan, you first get another catscan and then immediately following that, you are rolled into an attached petscan machine right behind it and you stay in one position for 5 minutes (as the machine counts the gamma rays) and then it moves you about 8-10 inches and then you stay in that position for 5 minutes (again it counts gamma rays) and this continues for about 30 minutes overall. Your arms are extended over your head for the 30 minutes. The purpose of the catscan is to show where your organs are and then the petscan image is overlaid on the catscan image and thus the technician can see where the glucose is being absorbed relative to your insides. The gamma ray detector in the PETSCAN machine is under you during the imaging. Click here for more details on pet-scans.
Below is an image of the radiologists report from my catscan:

====================================================
Below is an image of the radiologists report from my combined catscan/petscan:

The Petscan looks quite good! There is no sign of unusual metabolic activity. Cancer likes sugar as it grows and thus it metabolizes it. Without signs of unusual metabolic activity, there is no sign of an active cancer (at the level the machine picks it up anyway).
====================================================
2/24/2007-I am in far better shape than I was back in the fall of 2006 (UGH!). Specifically, I have no tubes in me, I am off pain killers, I have no pain and can walk/run normally. From the view of a naive consumer of medical services, I am greatly improved and I am back in NYC this coming Tuesday (2/27) to see the oncologist for his interpretation of the cat scan and pet scan reports.
I was glancing at the March 2007 Readers Digest and on page 124, they have a small article entitled "A JUICY CURE FOR PROSTATE CANCER" and it basically says a study at UCLA found if one drinks 8 ounces of Pomegranate Juice every day, it significantly slows down rising PSA levels which help indicate the presence of cancer and more trials are planned. FYI: I drink this tangy red liquid every single day!
The one year anniversary of my surgery was 1/17/2007 and below is a picture of my scar on that date and you will also see two bags (one of each side of me) - these are bags that are connected to my kidneys as of that date. The idea was to give my bladder a rest and it worked. Also, notice how the surgical scar is fading - the surgical team did a stellar job in that I will soon have NO scar at all and this was MAJOR surgery according to them.

====================================================
02/28/2007
As you can imagine, I have a lot of medical supplies at home, what with prescription drugs, bandages, face masks, stethoscope, breathing exercise equiment and so on. Here is a picture of just some of my supplies (I have many more supplies not in this picture):

02/28/2007-We met with the Oncology doctor yesterday and we discussed the catscan and petscan and he said they look quite good, i.e. the tumor is still there but has stopped growing and thus may be either dead or stunned. For now, there is no other plan for treatment but he will present my case on Monday to a multidisciplinary group of oncology doctors, radiation doctors, urologists, etc and come up with a game plan, i.e. perhaps localized radiation. He cautioned only 1 person out of 999 in my situation are cured so expect it to come back, perhaps in my joints, ribs or my brain. But he also said he will monitor me and catch it before I likely feel it (using periodic catscans, the first of which is in 2 months). He also gave me the okay for local driving and I can travel but I need to watch my stamina as I am still weak. He also ordered an infusion of Zometa (4mg in 100ml of dextrose). This helps with bone formation and my cancer was pressing against a (pelvic) bone. Zometa will help repair it.
I should add I have NO pain anywhere and my bladder is working fine and I can walk fine (compare this to December!). The main issue remains stamina, i.e. I go up the stairs and I am out of breath. But I know my stamina will come back. I calculate I was in the hospital (overnight) some 20 days (just shy of 3 weeks) and I also was in the Emergency Room some 5 times and 4 of these times I was sent home after treatment. These 20 days and 5 ERs are [largely] what affected my stamina but also I have been quite immobile at home for some weeks (by necessity) and that also weakened my stamina. So I hope to take some daily walks as well as go up and down the stairs to rebuild my stamina and it will take a few short months I guess.
2/28/2007-I drove solo for the first time since 9/10/2006 and it felt great!! I drove perhaps 20 miles in all and will do the same tomorrow as well.
3/1/2007-But that drive did tire me quite a bit....I was in bed at 8pm and out for the night by 930pm. But I will do it today again to build stamina.
3/3/2007-I do not need to rest each afternoon anymore (I used to lay down for 2-4 hours each afternoon) so my stamina is getting better. Sleep has been mildly problematic, i.e. I usually wake up at least once in the middle of the night, quite thirsty; I drink some water and then back to sleep until 7am or so.
Also, I was looking at the book Pathophysiology (4th Edition, 2002) and on page 752 it says the 5 yr survival rate of all stages of prostate cancer is up to 92%, 10 years is 67% and 15 years is 52%. These are 2002 numbers and it can only be better here in 2007.
3/7/2007-The oncologist called me yesterday to say the group of doctors met on Monday and decided radiation therapy makes sense at this point for me and he said this could be a 'home run' for me. The plan is 5 days of radiation per week, for 4 weeks. I asked re the danger to adjacent areas (colon, rectum, bladder) and he said the radiation would not be too intense as he understands it. I meet with the radiation oncologist on 3/22 to discuss next steps.
3/9/2006-I came across an interesting article in a Readers Digest magazine. Below is an excerpt (you can see the full article on www.rd.com/vitamin) (bolded text in the body of the article is done by me):
D Deficiency and Certain Cancers
Some of the stunning findings: Getting 1000 IU (international units) of vitamin D from supplements or the sun may cut the risk of colon cancer in half, a change that would save many thousands of lives every year. Increasing vitamin D intake to 2000 IU would reduce the risk by two-thirds, says epidemiologist Cedric Garland of the University of California, San Diego. In 1980 Dr. Garland and his brother Frank, also an epidemiologist, published a groundbreaking study showing that rates of colon cancer were about twice as high in the sun-starved northeastern United States as they are in the sunny South.
Since then, evidence of the connection between vitamin D deficiency and cancer has strengthened, prompting researchers to make some startling claims. Considering all types of cancer, insufficient vitamin D trumps the other risk factors, says Dr. Garland. Of course, for certain cancers some of those "other risks" are overwhelmingly powerful. For example, vitamin D won't stop some smokers from getting lung cancer or heavy drinkers from being at risk for oral or esophageal cancers.
But researchers have now identified at least 18 types of cancer that are more common among people who don't get enough vitamin D, including such common ones as breast, lung and prostate. (Other cancers that have been linked to vitamin D: bladder, esophageal, gastric, ovarian, rectal, renal, uterine, non-Hodgkin's lymphoma, cervical, gallbladder, laryngeal, oral, pancreatic, Hodgkin's lymphoma and colon.) They've learned that prostate cancer typically strikes men who work indoors four years earlier than it occurs among men who work outdoors. And they suspect that higher rates, and more aggressive cases, of prostate cancer among African Americans occur because black skin doesn't efficiently absorb the ultraviolet B (UVB) rays that trigger vitamin D production. In Africa, black skin does a great job of absorbing UVB. The weaker rays farther north just don't make it through often enough, leaving African Americans more likely than whites to run low on vitamin D. The same thing may explain why breast cancer tends to be more aggressive and more frequently fatal among African American women than it is among white women.
Can Vitamin D Cure?
Even after cancer strikes, the vitamin D our bodies make in the summer helps fight the disease. A study at Harvard found that mortality rates were 40 percent higher among lung cancer patients operated on in the winter than among those who had surgery in the summer and had high levels of D from sun or diet. This year, a British study found that survival rates there are highest among cancer patients diagnosed in the summer and fall. And last year in Norway researchers found higher survival rates among young people with Hodgkin's lymphoma diagnosed in the autumn.
Benefits aren't limited to D from the sun. In Canada, patients given vitamin D along with chemotherapy had fewer side effects and developed fewer thromboses (blood clots), serious complications of treatment, than those who got a placebo with chemo.
How can a mere vitamin harbor such amazing powers? For starters, D isn't really a vitamin. In the body, it is transformed into a benevolent hormone, shoring up our bones, regulating cell growth and helping prevent the kind of wild cell proliferation that leads to cancer. "Almost every tissue and cell in the body has receptors for vitamin D, which means that every tissue and cell needs vitamin D to function maximally," says Michael F. Holick, MD, a vitamin D researcher at Boston University.
In the lab, researchers have watched as activated vitamin D actually turns off cancer. When prostate cancer cells were exposed to D, the cells stopped reproducing wildly and resumed normal, orderly growth. Later studies showed that the same process occurs in colon and breast cancer cells. And when Dr. Holick's team gave vitamin D to mice with colon cancer, they witnessed a 40 percent reduction in tumor growth.
The big challenge now? Distilling the cancer-protective elements of vitamin D into compounds that can be used to treat humans.
The same message was also found in an issue of Cancer Research (6/15/2005) and I except it below "A study was published in the June 15, 2005, issue of Cancer Research regarding sun exposure, vitamin D receptor (VDR) gene polymorphisms, and risk of advanced prostate cancer (PCa). This population-based, case-control study was conducted among non-Hispanic white men ages 40-79 from the San Francisco Bay area. The researchers found that reduced risk of advanced PCa was associated with high sun exposure, and that significant reductions in risk of advanced PCa was found among those with high sun exposure and VDR polymorphisms (ORs ranging from 0.46-0.67 for various genotypes). The authors concluded that sun exposure and VDR polymorphisms play an important role in the etiology of PCa."
3/23/2007-I just came back from a week in Florida (West Palm Beach, Deerfield Beach and Boca Raton areas)and the sunshine there (80 F every day) did a world of good for my health, i.e. I developed a light tan and this makes Vitamin D. Also, no stairs in Florida per se so easy walking and I spent every day at the beach (but did not swim due to stamina issues).
I meet a radiation oncologist today (NYC) and then my oncologist next Tuesday and they will start 4 weeks of radiation shortly thereafter and that may kill any cancer left in me. Right now it is felt to be dead or stunned or dying and there is no signs of spread. It is the size of a small potato in my left hip area but I do not feel it. Back in the fall, I could barely walk due to pain in my left pelvic area and my wife thought I might die before the end of 2006....but I am the picture of health now!!! Thank you Florida sunshine!!
3/25/2007-we met with a Radiation Oncologist and he impressed us greatly so we will use him. He asked we do a simulation first, i.e. so he can find the tumor and mark my body accordingly. He felt my tumor will not move around (it is attached to left hip bone) so we need not be as concerned as we would be if it was attached to my colon which does move freely in the abdomen. I indicated my left hip might be weakened from cancer and he said he would talk to an orthopedic doctor about my case (this doctor had clearly been briefed about me before we met). I also mentioned he was referred by my Oncologist and I also gave him my urologists name. I went to this radiation oncologist because all my medical records are in this building and all my doctors are in this building. I was going to request a referral to a radiation oncologist closer to home but this doctor impressed me enough I will use him. Stay tuned.
3/27/2007-Today was a long day at NYP; I first met with Dr JosephL (the head of the Orthopedic Dept at the hospital); this was a referral from Dr BhupeshP (and earlier, Dr EDV). Dr JosephL first watched me walk and then he flexed my left leg (where the prostate cancer was previously pressing against the left pelvic bone). He said I am okay for radiation therapy (Dr BhupeshP is the radiation oncologist who had the concern - too much bone loss and he cannot safely do radiation treatment). Dr JosephL also said I am to avoid all impact activities, including a treadmill (and of course basketball, tennis etc) but I am okay for regular walking and any activity in a swimming pool. These restrictions are likely for the rest of my life and are a direct result of the cancer earlier damaging my my left pelvic bone and invading it somewhat - lucky for me, I am not sports-oriented and I just love to walk.
I then met with my Oncologist (Dr DavidN) and he said I am to see him right after Radiation treatment finishes. He also said I look great overall. I asked if it makes sense for more chemo either during radiation treatment or immediately after and he said no. I did get a blood test while I was with Dr DavidN and my RBC was a little low. He also said no dental surgery as I am on Zometa and one cannot have any dental surgery within 3 months of taking Zometa. (Zometa helps strengthen bones).
I then went to see Dr BhupeshP to get lined up for radiation treatment. His team had me lay me down on a machine which allowed them to image me. First they did a fluoroscope to line me up. Then they took an x-ray, aimed straight down on my pelvic area and then another 90 degrees rotated counterclockwise. At that point they marked me up with a sharpie. Then they tattooed me (three very small pinpoint marks) and then they glued two small metal disks (much thinner/smaller than a penny), one on each thigh. This was to allow the cat scan to easily image the marks. Next I was given a stepwise cat scan. Specifically, they carefully had me lay down on another table with markings on it, much like a ruler. They spent some 20 minutes making sure I was carefully positioned, relative to my sharpie pen marks. They had to have me aligned within 5 mm(!). Then they started the CAT scan but it was not the usual smooth cat scan where they roll you in and out in 2 minutes or so. This was moving me in and out in stepwise increments so it took perhaps 5 minutes. The CAT scan technician then showed me the CAT scan image - I could clearly see the tumor (now quite calcified, i.e. it looked like a bone mass). Once this CAT scan was done, we went home. We go back this coming Wednesday (4/4) to discuss the treatment plan with Dr BupeshP.
4/4/2007
I went to the dentist today (for the 1st time in many months) and they remarked my teeth are okay and no problems per se. So I had a teeth cleaning and go back in 3-4 months. I then went to NYC to see Dr BhupeshP and first they double checked my tattoos and all looked fine and then he outlined his treatment plan which he said may be refined further yet. He showed us the IMRT plan via CAT-SCAN images on the computer screen and we could see the tumor readily - it was about 4" long or so and clearly calcified and no sign of growth etc.
4/7/2007
As I mentioned above, it has been decided I will soon commence radiation therapy. Radiation therapy is the treatment of cancer with ionizing radiation. Radiation works by (powerful (x-rays and possibly (even more powerful) gamma rays) damaging the DNA (genetic material) within the tumor cells, making them unable to divide and grow. Radiation is often given with the intent of destroying the tumor and curing the disease. However, although radiation is directed at the tumor, it is inevitable that the normal, non-cancerous tissues surrounding the tumor will also be affected by the radiation and therefore damaged. The goal of radiation therapy is to maximize the dose to tumor cells while minimizing exposure to normal, healthy cells in the area near the tumor cells. The intensity of (external) radiation a patient receives is measured in a unit known as Grey units. Grey units are sometimes referred to cGY, i.e. 1/100th of a Grey Unit. My understanding is that Radiation Therapy will use X-rays and/or Gamma Rays in the mega-electron-voltage range, produced by a linear accelerator. The specific energy is in the 4-25 mega-electron volt range (powerful penetrating x-rays/gamma rays) and can penetrate deep into the body when needed. The x-rays/gamma rays will hit atoms in the tumor cell, kick off an electron which then ionizes it and damages the tumor cell. Cancer cells often cannot recover from this while normal cells can usually repair the damage.
Intensity modulated radiation therapy (IMRT) is one form of Radiation Therapy and creates a shaped radiation beam, delivering high doses of x-ray radiation to the tumor and significantly smaller doses of radiation to the surrounding normal tissues. This may result in a higher cancer-control rate and a lower rate of side effects. IMRT has been used successfully in the treatment of several types of cancer, including prostate, cervical, nasopharyngeal, and pediatric cancers. With IMRT, varying energetic doses can be sent from different angles and all these beams intersect in the tumor area and these individual smaller doses add up to the desired impact in and around the tumor while lessening the chance of damaging areas near the tumor (each individual smaller dose generally does not hurt normal cells).
Anyway, I will get 1.8 Grey units for each dose. Each dose is once per day and usually takes about 5 minutes to administer. This is 5 days per week and then the weekend off to allow my body to rest from it. The total dosage received over time is also important, i.e. I will likely receive between 50 and 60 Grey Units over the course of treatment. The tentative plan is 8 doses across my lower abdomen and then some 15-25 doses targetted at the tumor itself (using IMRT techniques). Changed, see 4/10/2007
The more common side effects of radiation therapy can include nausea, diarrhea, a burning sensation when urinating, skin irritation and fatigue. Less common (less than 10%) side effects can include a bowel obstruction requiring surgery.
After Radiation Therapy, my oncologist wants to see me and I will likely get another cat scan or pet scan to see if any cancer is left in me and also to see how the tumor has changed as a result of radiation. I may in fact get some more chemotherapy after radiation therapy just to be sure the tumor is dead.
I think this will all be less of an impact than Chemo which was tough on me on many levels. Stay tuned. As of today, it starts Tuesday. Changed- It starts Wednesday (see 4/10 for details).
4/8/2007
Summary of period 9/10/2006-1/30/2007:
* I lost some 20% of my body weight (between 9/10/2006 and year end 2006)
* I had some 7 Emergency Room visits (between 9/10/2006 and 1/30/2007) in three different hospitals in two different states.
* In all, I spent some 24 days in the Hospital (1/1/2006-12/7/2006, 20 of which were unscheduled.
* I had some 15 days of chemotherapy via IV Infusion ( 9/10/2006 through 2/8/2007)
* I had countless X-rays (15?), blood tests (50-75?)
* I had countless IV tubes put in me (40?)
* I had 4 cystoscopy procedures (since 9/10/2006)
* I was given 6 units of blood due to tremendous blood loss (11/25/2006).
* I am given countless doses of prescription drugs, some are quite expensive indeed!
* I have kidney tubes in me some 70 days
* I had a Foley Catheter in me for some 73 days
* Numerous tests: cat scans, pet scan, bone scans, MRI, Bone Density scan, X-Rays etc
Let's hope all this is behind me now! I drive now, walk the dog etc. Except for stamina issues, I feel fine.
4/10/2007-We went to the radiation center and they had me get in hospital gowns and then then x-rayed me from many directions. I was on my back and they took one x-ray straight down and then one from the left and then one from the right and then one 45 degrees up the horizontal on both the left and right. All during this, they made sure I was lined up exactly on laser beams, i.e. the lasers were pointing right at the tattoos. This allows repeatable images to be made and thus they can see if the tumor has shifted (it is not expected to). Then we met with the Radiation Oncologist and he stated I will get 1.8Grey units (see above) per visit and it will be aimed at and near the tumor and use IMRT techniques. It starts on 4/11/2007 and ends around 5/11/2007 but even without radiation after 5/11/2007, the cancer cells will die for another month or so (Radiation breaks their DNA and cancer tries for a few weeks to fix it and it cannot so it simply dies). All the radiation will be aimed squarely at the tumor and perhaps 1/2 to 1" around it. Care is being taken to minimize radiation to nearby organs (rectum, colon, bladder, gonads, etc) as part of this. In early June I meet with the Oncologist and schedule a cat scan/pet scan to see what is going on. He also said I will feel the effects of radiation not right away but towards the end of treatment, i.e. fatigue, nausea, etc and each person acts differently. He is quite confident with this plan:

==================================================================
4/13/2007-Today is the 3rd day of radiation treatment for me. To make it easier for me (my wife cannot take off from work all the time and my wife also says my driving skills are not back yet sufficient to drive to NYC every day), I take a bus into NYC's Port Authority Bus Terminal and then the #7 subway to Grand Central and then the #6 (north) to the Hunter College stop and then exit and walk to the East river (4 blocks). I arrive at the radiation department and when it is my turn, I change from my street clothes into a long hospital gown. But I only need to undress from the waist down as radiation is aimed just below my waist. I undress for two reasons, i.e. (1) so the radiation therapist can see my three tattoos (for laser alignment) and (2) by removing my clothes, I also remove any metal (belt buckle, metal buttons, zipper, etc) which could interfere with the x-rays.
Anyway, then I am asked to follow the therapist who takes me into a room where there is a linear accelerator machine (made by Varian Corporation). The machine (known as an IMRT machine) can emit normal x-rays to take standard x-ray pictures or more powerful x-rays to kill cancer cells. I lay down on a table (blankets below me and on top of me to keep me warm. The therapist positions me carefully on the table, essentially to literally the exact same spot each time (in this room they have wall and ceiling mounted lasers that aim at the patient, me). They simply position me such that the lasers are aimed at the small tattoo marks on me from my 1st visit. Once I am properly positioned (within 1/2 millimeter), the therapist tells me to lay very still (even talking may move me slightly) and he leaves the room and closes a heavy door behind him. The door weighs many tons (has lead metal in it to protect the therapists who use the machine all day long). Once that door closes and seals, the therapist activates the IMRT from another room, according to a plan put together by the radiation oncologist and the physicists on the staff. This plan tells the therapist how many doses I am to receive, from what direction and how wide a beam to use on each dose. In my case, I receive doses from 6 different directions, all aimed at the tumor itself. Since only the tumor is the common target of all 6 doses, it is impacted the most - the rest of me generally gets just one minor dose as the target from all directions is the tumor. The intensity of the beam is as high as 15 MEV on each beam and it ends up being 1.8 Grey units of energy overall for all 5 doses. While this is happening, the therapist is in another room, and he watches me from a camera and we can talk to me via a microphone/speaker mounted in the room. The IMRT machine rotates around me between doses and when I do get a dose, a loudish hum is heard. Each dose lasts about a minute or so.
Once it is over (10 minutes?), the door opens and the therapist comes in to assist me off the table if needed. I get up, thank him and walk back to the changing area and put on street clothes and then head home to rest.
Below is an IMRT set up in a room and this is quite similar to what I was seeing in the room where I received my radiation treatment.

===================================================================
Below is a schematic showing the insides of an IMRT machine - basically, the machine makes high energy x-rays (by shooting high speed electrons at metal and this generates x-rays) and then aims them out the imaging window at the patient.

===================================================================
4/15/2007-A catscan takes multiple x-rays of the target area, i.e. one 'slice' at a time and each a slightly different area. My own catscans tend to take 100+ x-rays and below is from slide 92 of 107 x-rays on 2/21/2007 and I have circled in red the approximate tumor itself. If you click on the image, it will show you the image full size. The tumor looks somewhat like a bone as it is turning into a bone structure as it becomes necrotic (dies). The bones should be symmetric around the center of the image, i.e. left and right side bones should be symmetric and clearly they are not. The Cancer damaged/destroyed part of the bone on the right in this image before the cancer itself starting becoming necrotic. Chemo stopped the cancer and radiation, now underway, will hopefully finish it off.

Back to top
4/20/2007
Here are numerous images showing details on my radiation treatment. I have had my first full week of radiation (5 days) and three days from the prior week so 8 days in all. The good news is one of my sisters was once a senior radiation therapist and 20 years ago trained 3 of the people who work at the facility where I get my treatment. So they know me well (via my sister). Anyway, here are the images, starting with the 7 pages of the detailed treatment plan.
==============================================================

==============================================================

==============================================================

==============================================================

==============================================================

==============================================================

==============================================================

==============================================================
Now we have two more images. The 1st shows images of my lower abdomen with outlines of the cancer itself and additional outlines of where the radiation will hit and the angles it will come in at:

==============================================================
This image shows the impact of radiation on various nearby organs. These two images are put together with the physicists on the staff at the radiation oncology department and they decide (with the doctor's input) which radiation, how much, from what direction and so on. The prior image and this is from that team.

==============================================================
4/22/2007-Battling a major illness or Cancer
My Tips for Battling Cancer (or a Major Illness).
If you have just been told you have cancer (or another illness) by your doctor, do NOT despair or get upset. Cancer occurs when your body's cells stop dying and just keep dividing endlessly. Cancer was once a deadly killer but these days there are many people who have beaten cancer. The important step now is to approach it carefully and aggressively. I list below some tips you should take to beat cancer (or any serious illness) and I hope they do help you. These steps below come from my personal experience battling prostate cancer as well as some research I have done and also conversations with doctors. Here are some specific steps I suggest you consider:
1)-Get smart on your specific cancer (or illness). Breast cancer is not pancreatic cancer and skin cancer is not brain cancer. Each cancer is different and there are even subtypes of cancers. For example, I have an unusual form of prostate cancer and not your typical type of prostate cancer. Anyway, get smart on your type of cancer using the web or other resources. Ask the doctor what type of cancer you have. Ask him how its progression is measured, i.e. for Prostate cancer, a biopsy will have a Gleason Score of 2 through 10 and the cancers progress is measured via its t-score (T1, T2, T3, T4). Your cancer may use a different scoring (the Scarff-Bloom-Richardson system is one such system) so ask your doctor some questions (1) is this cancer confined to where she or he found it or has it spread elsewhere (2) is this cancer slow growing or aggressive (3) how does it score on a scale like the Scarff-Bloom-Richardson scale and so on. Once you know, start searching the web and I suggest you start with these web sites:
National Cancer Institute: http://www.cancer.gov
American Cancer Society: http://www.cancer.org
National Institute for Health: http://www.nlm.nih.gov/medlineplus/cancer.html
2)-Tell everyone you know RIGHT AWAY. They or someone they know may have already done the research and thus may know great doctors and/or hospitals. Don't be shy, tell everyone! I did this and found a VERY GOOD SURGEON at a VERY GOOD HOSPITAL, just because I spoke up & told many people. One of the people I told had a coworker who had just went through what I went through and told me of this great doctor and that is who I chose for surgery. Another person plays golf with the head of radiation therapy at another hospital - you get the idea – so tell everyone!
3)-You may have to decide your approach between the three major approaches to cancer, i.e. surgery, radiation and chemotherapy (I have had all three!). Surgery is very specific and the surgeon will likely miss microscopic cancer cells. Chemotherapy hits your whole body and may kill 99.9999% of your cancer. Radiation can get the rest of the cancer if it is localized to one area. Each doctor will have his preferred approach just so you know, thus a surgeon will prefer surgery as one example. One caveat, once you have radiation, surgery is not so easy to do (due to scar tissue from the radiation). Radiation can mean many things just so you know, i.e. internal radiation, external radiation etc. Chemotherapy usually means strong toxic drugs to kill cancer but could also mean inserting some genetically-modified cells into the cancer to kill it. Anyway, try to decide which approach works for you. In my case, I opted for surgery 1st as my cancer was fast moving (high Gleason score and high T-score) and I wanted as much out as possible right away and then I needed chemo when it came back and then radiation to finish it off.
4)-Pick your doctor and hospital carefully. The nearest hospital may not be the best hospital for you. Do they perform surgery, radiation and chemotherapy every day or just 4x per year?? Get a doctor/hospital where they routinely do this treatment perhaps even weekly and preferably a teaching hospital. Each year, US News & World Report magazine surveys doctors to find the best hospitals in the USA. Visit the below links to help in your search.
TOP RANKED HOSPITALS OVERALL:
http://health.usnews.com/usnews/health/best-hospitals/honorroll.htm
TOP RANKED CANCER HOSPITALS:
http://health.usnews.com/usnews/health/best-hospitals/search.php?spec=ihqcanc&
Also, try these two links as well:
COMPARE HOSPITALS: http://hospitalcompare.hhs.gov
CHECK EACH STATES LICENSING AND DISCIPLINARY DATABASES: http://www.fsmb.org/directory_smb.html
My sister is a former radiation therapist and she adds that the hospital you select should be a multidisciplinary facility. Thus the medical oncologist will meet with the surgeon and the radiation oncologist to decide the next steps for you, the patient-they work together for your benefit. I would add you also may want a teaching hospital and that also conducts clinical trials.
5)-Keep a diary of everything that happens as it WILL be a real blur after a period of time. I kept a diary and then I moved it to a web blog (http://prostate-cancer-log.blogspot.com). I urge you to write EVERYTHING down (how you feel, what test you had, sleeping problems, drugs taken, etc). Date each entry as well (obviously). My diary has been a lifesaver for me on many levels. I kept it with me at every meeting with the doctor, by my bedside at night and when I was in the hospital, I kept it nearby so I could write down what was going on. I have a paper diary and the blog is derived from my paper diary.
6)-Ask your doctor AND the hospital for copies of all medical tests, i.e. your biopsies, tests, blood tests, cat-scans, bone scan, pet-scans, MRIs etc. Ask for it within 3-4 weeks of having the test. They will not offer it to you - you have to ask. If you wait too long, it may become unavailable (archived). These copies will be invaluable later on. I also copy the CDROMS they may give me to my computer and I scan any papers to my computer. It is normal for a hospital to charge for making some copies, especially of images of x-rays, bone-scans, cat-scans, MRIs pet-scans and so on. Radiologist reports from those images are generally free for the asking. Generally speaking, you want both the images and the associated radiologist reports.
7)-Whenever you meet with a doctor, have another person come with you and this person's role is to bring a notebook and write down what the doctor says. You will be the person having a conversation with the doctor and thus you cannot write down what he or she says (too distracting to the doctor).
8)-Keep a positive outlook. Say every day that you will beat cancer. Attitude is perhaps 50% of the reason people beat cancer. With the way science is making breakthroughs, very soon your cancer will be under better control and finally beaten. I know many people who beat cancer and all had a positive attitude.
9)-Prepare a one-page summary of your health. I went to the emergency room 7 times between Sept 2006 and Jan 2007 and quickly realized having a one-page summary is handy to have for the ER team. Do NOT put your name or date of birth or social security number on it but do put your blood type and a summary of what you have gone through thus far, including recent blood tests (and dates) as well as dates of chemo, cat scans and so on. I also track when I was in the hospital, emergency room, date of last chemo, last radiation etc. It has been very helpful to me. I keep my cell# on mine in case I lose it or the doctor wished to call me.
10)-Review your eating habits. One senior doctor told me it was something in our diets that gives us cancer or at least makes it easier for cancer to start. In the book DR. PETER SCARDINO'S PROSTATE BOOK, the author (Dr. Scardino) states (page 96) "The evidence for a nutritional link is compelling". Having read this, I researched it and found these books that helped me-I have read them and they are quite good. The first is called "BEATING CANCER WITH NUTRITION" by Patrick Quillin. Get it from your local library or buy it online or at your local book store (I purchased used copies on Amazon.com). The current edition came out in 2005 and its ISBN# is 978-0-9638372-9-5 (your library may need this number). The second book is called "HOW TO PREVENT AND TREAT CANCER WITH NATURAL MEDICINE" by Dr. Michael Murray. This book came out in 2002 and its ISBN# is 1-57322-343-3. A third book and perhaps the best is FANTASTIC VOYAGE by Ray Kurzweil-(ISBN: 1-58954-954-3, 2004). I STRONGLY recommend you read these books, especially “Fantastic Voyage”.
NOTE CAREFULLY:
I am NOT a medical professional and thus this is only my personal opinion and only you can decide if these tips work for you.
You can download a copy of this (in Microsoft Word format) by clicking here.
==============================================================
I hope the above helps you in some small way and good luck
Back to top
4/23/2007-Some have asked me re drinking pomegranate juice, i.e. it is expensive they say. Actually, if you look around, you can find 100% pure pomegranate juice in many places (better fruit/vegetable stands, Trader Joe's etc). When you find a pomegranate juice, just be sure it has nothing else (read the label carefully). It is okay if from concentrate and purified water but that is all as I want the pure stuff and so do you. Below are some photos of some common pomegranate juice bottles. Pom Wonderful is good yet pricey (16 ounces for $5 or so). You can readily find 32 ounces for $4 if you hunt around. The other three bottles are 32 ounces and I think I paid $3.97 or so for each of them. Hope that helps. Again, my urologist drinks it and everyone I know who has battled a serious illness drinks it also and all are quite healthy today, including me.




==============================================================
4/26/2007-I completed 12 days of radiation and it goes smoothly. It also helps me regain my stamina as I drive to a bus stop, ride the bus into NYC, ride 2 subways (#7 and then the #6) and then I walk 4 blocks to get to the hospital for radiation treatment and then I do the reverse trip coming home. I am a bit tired from it but that tells me I am pushing myself the right amount. While at the hospital, I stumbled on this brochure and I wanted to share it with you (click on any picture in this blog and it will expand it so you can read it or see more detail).


4/29/2007
I am sitting in a small waiting area, waiting my turn for daily radiation treatment and the man sitting to my left (wearing a turban typical of people in India) says to me "Does it always rain like this?" (it had been raining hard that day) and I said no and when did you arrive from India? He says I just found I had cancer and promptly flew to America to this city so I could get treated at this hospital .... that says it all - this (NY Presbyterian Hospital at 68th st and York Ave) is a great hospital indeed, ranked #6 in the nation per US News and World Report's survey of doctors.
I need to track my progress in rebuilding my stamina so I use a great pedometer (Omron HJ-112)and it track my steps each day and also how many miles that is and how many kilocalories I have consumed. It appears I walk between 2 and 5 miles per day which is good for me. The pedometer costs about $25 at Target stores and I just keep it in my pocket as I walk around. Here is a photo of it:

==============================================================
4/30/2007
I met with the Radiation Oncologist and asked about my diet (see 4/4/06 above) and how it may impact radiation treatment and he said that it would be wise to stop drinking my daily mix as it is loaded with potent antioxidants that will likely sweep up some of the free radicals created by radiation and the free radicals help kill the cancer. He said this is his opinion only and stop only while I am getting radiation. So I stopped effective today - what I did was stop all dark liquids (grape juice, blueberries, pomegranate juice) for now.
5/1/2007
It hurts today to urinate (it hurt less yesterday). This is after 15 doses of radiation. The Doctor today took a urine sample and also prescribed flomax. My sense is my bladder and urinary tract are still quite sensitive after:
*Radical retropubic prostectaomy surgery on 1/17/06 (when 1/3 of my bladder was removed due to Cancer) and then the many problems of last fall and winter (9/10/06-2/8/07), i.e.
*Numerous bladder blockages (due to blood clots).
*7 emergency room visits,in 3 different hospitals in 2 different states.
*Countless bladder spasms.
*4 cystoscopy procedures via my uretha.
*73 days with Foley catheters.
*70 days of bladder bypass (via kidney tubes).
*7-10 days of bladder irrigation to get bladder bleeding under control.
*Losing some 6 units of blood via heavy bleeding in my bladder late last year. (late November).
*20 unscheduled days in the hospital last fall as a patient due to cancer hitting my
bladder and causing all these problems.
*Included in all this is 3 doses of Taxotere (chemo) and 4 doses (each given
over 3 days) of Cisplatin and Etoposide (more chemo), some 15 days in all.
I will see what drinking lots of water does for me (doctor's recommendation) and also flomax. He also wants to see me on Friday and may give me a few days off from radiation.
5/2/2007
The Radiation Oncologist called last night and said based on what my bladder and urinary tract have been through (see 5/1/07), let's give my body a few days rest so no radiation Wednesday or Thursday this week and depending how I feel, none on Friday and then normal dose resumes on Monday. I am feeling better and drinking lots of liquids. I am also about at the 1/2 way mark on radiation treatment, i.e. 15 doses thus far and about 15 to go (27 Grey units so far out of 54 expected).
5/4/2007-The pain I was feeling when I urinate is slowly going away. I do drink lots of water and that seems to help. Also, see the two books I added for 4/22/07. It is item 9 on that date.
5/8/2007-I resumed radiation yesterday (the pain from urinating was largely gone) and also met with my urologist (Dr. EDV) and he said it is likely my urinary tract (the urethra section-the tube connecting the bladder exit to the point urine exits the body) is inflamed (and not scar tissue) and he asked for a urine sample and said he may wish to look in the urethra next week. I then met with a radiation oncologist yesterday and he examined me and did not see anything wrong and did say my urinary pain is likely radiation causing inflammation in the uretha. I then received a dose of radiation and came home. Today I went back again and let them know it hurts more and I also have 'urinary hesitation' which means I tell my body to 'pee' and it takes 1-2 seconds for it to appear. He said he may add more flomax to the prescription, i.e. every 12 hours instead of every 24 and I asked him re taking Chamomile tea to help with the inflammation and he said to give it a try, it may help. Then I had another dose of radiation and came home...at least I am more than 1/2 way through the proposed radiation treatment plan. Below is my (poor) attempt to show a normal urethra section and then an inflamed one. My inflammation is partially closing off the urethra tubes and that explains the pain and the urinary hesitation I notice:

===================================================
5/11/2007-The Flomax seems to be working and my radiation oncologist said it does take about a week to kick in. The pain is largely gone and it only hurts when I start to urinate. I still have some minor urinary hesitation but I can live with that. They took another blood sample today to monitor my blood chemistry etc. My last blood test was on 4/26 and showed these values:
WBC 2.3
RBC 3.5
HemoGlobin 12.0
Hematocrit 34.6
All these numbers are low and thus they took another blood test today.
* I also had some urine samples taken and these came back normal. They did this test to make sure I did not have an infection in my bladder system. My Urologist may look inside my urinary tract next week to inspect the inflammation as it is likely near where he did that major surgery back on 1/17/2006.
* As of today I am about 2/3 done with Radiation Therapy, i.e. today was dose #20 and I believe I get 30 or 31 doses. I expect about two more weeks of this (5 days/week).
* After all I have been through, it feels so good to be able to walk, go up and down stairs, to ride buses/subways and just feel the warmth of the sunshine. Having had a tough battle with cancer gives you a new appreciation for life! You enjoy every minute of every day and appreciate the beauty of singing birds, a thunderstorm, stunning flowers, a passing car, the stars at night, your pets etc. You look at every person from a new perspective also. Every new day is truly a brand new gift, to be carefully unwrapped and enjoyed to its fullest.
5/16/2007-The Urologist decided there is no need to look inside my urinary tract today so instead I had lunch with two good friends I have not seen for a long time; we had a lot of laughs which I need. Radiation is still hitting me every day but side effects are largely unchanged (see below). The Radiation oncologist said he may extend radiation a few extra days. I am overdue for a lupron shot and that will likely happen this week.
My blood test on 5/11 came back and here are the numbers:
WBC 2.5, was 2.3 (last week)
RBC 3.5, unchanged
HemoGlobin 12.1, was 12.0
Hematocrit 34.8, was 34.6
These numbers continue to be low but the doctors are watching it. I also have what looks like a bad case of sunburn on the surface of my skin in the left pelvic area (above where the cancer tumor is). I called the Radiation team and a nurse told me to put RadiaGel on it and that did help. But not to apply it before radiation tomorrow. The Radiation Oncologist had told me some weeks ago this could happen from the radiation and wants to see me tomorrow to look at the redness.
5/18/2007-The radiation oncologist looked at the redness and said this is normal and said I should put some Radiagel on it 2x/day. He also said there are about 6 more days of radiation for me and then I am done. I then went to the urology department and they gave me a new dose of lupron - I receive this every 3 months or so. They also lent me a very good book "DR PETER SCARDINO'S PROSTATE BOOK" by Dr Peter Scardino (trained by my urologist!). I am reading that now; I should add that my form of cancer is quite rare (UGH). Basically it is Small Cell Anaplastic Carcinoma of the Prostate, what this means is perhaps 1% of prostate cancers of this type- I'm so grateful I am getting treated at a very good Hospital by very experienced doctors.
5/20/2007-I tried Aloe gel from an Aloe plant we have (I broke off a leaf and used that to get the gel). I rubbed the gel from the leaf directly on my radiation burn and the next day, the skin was much smoother and less sensitive. I plan to try (commercial) Aloe Gel today. I also bought Scardino's book (see 5/18/2007) on Amazon for a total of $10 - a good deal for a great book.
5/23/2007-I am starting to see/feel the effects of radiation, painful to urinate, some minor bleeding from my urethra. This is after 28 doses (of 31) of radiation. The doctor said to go on flomax 2x per day and he may cancel Friday's radiation to give my body a rest. I bought a large ALOE leaf today - about 3ft long and PLENTY of sap in it. I rubbed some on the red area of the radiation and shortly thereafter, it calmed down nicely. I am off to VT this w/e with some good friends and I plan to relax as I need it. I also got the results of my blood test last Friday:
WBC 2.8, was 2.5 (last week)
RBC 3.68, was 3.5
HemoGlobin 12.6, was 12.1
Hematocrit 36.5, was 34.8
All these are below normal but improving.
5/29/2007-We went to Vermont for Memorial Day weekend and had a truly great time but the radiation side effects are still with me, i.e. fatigue, sunburn-like burn in the left front pelvic area and also on my buttocks...I need to apply Radiagel to them to cool them down. I also suffer from occasional loose bowels...all these side effects are unwelcome but expected after 30 doses of Radiation. I had dose 31 today and my doctor looked me over and said these side effects are expected at this point in my treatment which ends this week and it will take 1-2 weeks for me to bounce back from it. He also prescribed Silver Sulfadiazine cream USP (1%) as this is stronger than Radiagel.
5/30/2007-The Radiation Oncologist called me last night to say I am done with Radiation as I had enough to kill small cell cancers. I calculate I had 55.8 Grey units in all and all these Grey units have left me sunburned where the sun does not shine and fatigued as well. So I need to take it very easy this week as all those Grey Units have not yet taken their full toll on me yet. The doctor wants to see me next week and I am to see the oncologist (Dr DavidN) the week after.
5/30/2007-Here is my updated daily drink - it all goes in the blender and then I drink it as a main meal or one glass at each meal. Notice the rainbow of colors in the foods I use:
INGREDIENTS (in order I add them)
*1 heaping tablespoon of uncut raw organic flax seeds & then BLEND It (1)
*5 pitted Prunes (cut into quarters) – BLEND again
*1 packet of Revival Soy powder
1 pinch (< ½ teaspoon) of garlic powder
*1 pinch of cinnamon, oregano, tumeric gelcap and a dash of black pepper
*1 teaspoon of EVO (extra virgin olive oil)
*¼ teaspoon (level) of Baking Soda
*1 teabag full of green tea, cut open and dumped in & then BLEND it again
*1 peeled Banana (yellow)
*8 Ounces of Pomegranate Juice
*5-10 washed blueberries (fresh or frozen)
*3-5 washed Strawberries (fresh or frozen)-let it sit for 4-5 mins and then BLEND
*5-10 washed blackberries (fresh)
*5-10 washed raspberries (fresh)
5-10 washed dark grapes
*1 washed kale bunch (chopped up first)
*1-2 washed radishes (chopped up first)
1 yogurt container
1 slice of tomato
*Grape Juice and/or Orange Juice and/or Wild Blueberry Juice, to keep viscous (2)
*1 stalk of washed celery (chopped in 1/2) - use this to push kale etc down
½ stalk of washed carrot (chopped up)
*1 slice of white onion
NOW BLEND THIS MESS THOROUGHLY AND SERVE; makes about 3 tall glasses of a thick liquid.
*=these are the minimum set of ingredients, if possible
(1)=Flax seed is not digested by the body unless ground up thoroughly.
(2)=not too much as they have loads of (natural) sugar
I also take a multivitamin/multi-mineral pill with this. I do not drink tap water either- I drink water as pure as rain water, i.e. "purified" water. I also have at least one cup of tea (with both Green Tea and Celestial Seasonings Wild Berry Zinger in it) each day and also one glass of red wine each day. I also avoid all foods shown on at 4/22/07, item 9. Also, try to use the fruit/vegetables themselves instead of the juices as the juice tend to have a lot of (too much?) sugar
Later in the day, I have a V-8 with lemon juice and black pepper. I also have one glass of red wine. For dinner, it is often chicken and brown rice.
I plan to investigate Wolfberries (bright red) -[also known as Goji Berries] next. the goal is to have very wide range of fruits with deep colors in this drink.
I am sure this is far better than coffee and a buttered roll or toast. The point is, this smoothie (which I drink throughout the day) is simply packed with vitamins, nutrients and potent antioxidants. Raspberries and pomegranate juice are said to stop some cancers in their tracks (no scientific study in people yet but it does stop cancer in mice). Flax seed is somewhat like salmon and other fish, i.e. ALA, found in flax seed is the precursor of omega-3 fats, and can be converted to long-chain omega-3 fats and can therefore be substituted for many fish oils.
My Supplements
I take fish oil gelcaps (Nature's Way EFA Gold Mega Fish Flax Borage Olive Oil) , l-lysine pills (Country Life L-Lysine), curcumin gelcaps (NSI Tumeric with Bioperine) and Calcium Citrate pills (Nature's Way Calcium Citrate) every day and I have added Vitamin D-3 (Jarrow Formulae Vitamin D-3) to this list. You can buy most of these at a good discount at vitacost.com; by the way, I take Curcumin as studies show it likely kills cancer cells. I take the Fish Oil as it provides the right ratio of Omega 3 oils and Omega 6 oils (both essential nutrients the body needs). Same comment on L-lysine - the body needs this nutrient to work correctly. Vitamin D-3 is what the body makes when you are exposed to sunshine and some studies show it goes after cancer cells and kills them.
Back to top
6/3/2007-Today is NATIONAL CANCER SURVIVORS DAY (1st Sunday in June each year) and we went to a nearby hospital for a celebration with other survivors. It lasted some 2 hours and was a lot of fun! I next plan to look into RELAY FOR LIFE, another cancer survivor event. Regarding radiation side effects, I still have urinary pain and hesitation but the reddened skin areas are now tan and far less of a problem compared to a week ago.
6/7/2007-I sat outside yesterday and looked at the trees and then the puffy white clouds overhead and immediately a Joni Mitchell song ("Both Sides now") came to mind that describes clouds so well (the opening words) "Bows and Flows of Angel Hair and Ice Cream Castles in the air and feather canyons everywhere, I've looked at clouds that way". After battling cancer, I have a real appreciation for trees, chipmunks, our dog, shrubs, flowers, clouds, people, thunderstorms, the stars at night and life itself - all these things seem more intense to me now.
I did see my Radiation Oncologist today and he said I am tolerating radiation's side effects very well (good to hear) and stamina will take weeks to come back to normal so expect that. He also had a nurse draw blood (CBC) as a baseline to to speak. I left him and then stopped off at St Patricks Cathedral and said a prayer in thanks that I am winning against this rare aggressive cancer. I then came home and my Urologist emailed me that he wants me to get a bone density scan, probably to see the impact of Lupron on me. So that is secheduled on 6/12, the same day I am back in NYC to see my Oncologist. At home, my wife emailed me two GREAT links regarding foods:
http://www.cancertutor.com/Other/Big_List.htm
http://www.fruitarian.com/ao/FruitOnly.htm
Regarding my cancer's name ("Small cell anaplastic androgen independent carcinoma of the prostate"), this means (a) the cancer cells are smallish (b) anaplastic means they do not give off PSA as prostate cancer usually does (c) androgen independent means hormone therapy does not work on it and (d) the rest should be obvious.
6/10/2007-We see my oncologist on Tuesday and I also get a bone density test (an easy test) that same day in NYC. Then my wife and I head off to Naples Florida for a weeks vacation which she certainly needs after taking care of me when I was so sick. My medical situation as of now is: (1) it sometimes hurts to urinate still, (2) I still get tired easily. I did see two small clots (very small) when I urinated last night so I am cutting back on 81mg Aspirin and Vitamin E as both promote bleeding (slightly). I am hoping a trip to Florida will help me build up my stamina that much faster - the Florida sunshine was a BIG help back in March of this year!.
6/12/2007-I met with the medical oncologist (Dr DavidN) and he thinks I am doing well and look well. He warned me this cancer may well come back and contact him if I notice anything unusual. He then said he wants me to get a cat scan, pet scan and a bone scan in early July and see him again on July 17th. He also had blood drawn and my counts are a bit low, likely due to radiation treatments. I also met with my Radiation Oncologist and said my side-effects are expected and should go away soon. He asked to meet with me on 7/17 also. I also had a bone density test today for my urologist as he wants to monitor my bones as a result of Lupron therapy.
06/30/2007-I just came back from two weeks in sunny Florida where I largely relaxed every day and soaked up sunshine. Sunshine encourages your body to make Vitamin D (from cholesterol in the skin) which is known to kill some cancers. On Monday and Tuesday I am back at the hospital for more tests (CatScan, PetScan and a BoneScan). FYI: I love Florida weather!
07/02/2007-I had my bone scan today (results available tomorrow) and also received the results of my bone density test (6/12/2007) which shows a moderate risk of fracture due to bone density loss. This is not a big surprise since cancer damaged some bones in the pelvic area and Lupron is also known to cause some bone loss. I asked my orthopaedic doctor regarding restrictions and he said not to lift any package over 25 lbs (due to bone density issues)
07/03/2007-I received the report from my bone scan (yesterday and it (largely) shows just age-related trauma, i.e. sometimes my ankle hurts and so on. No new lesions detected. This appears to be good news. I had a cat/pet scan today and will have those results soon.
07/06/2007-I received the cat/pet scan reports via fax from the hospital and it looks fairly good, i.e. no hypermetabolic activity noted.
07/07/2007-NUTRITION TOPICS
NUTRITION GUIDELINES
"LET FOOD BE THY MEDICINE AND LET MEDICINE BE THY FOOD."
By Hippocrates, the acknowledged father of modern medicine
"THE HUMAN BODY IS THE ONLY BODY FOR WHICH THERE ARE NO SPARE PARTS."
by Hermann M. Biggs
"TAKE CARE OF YOUR BODY. IT'S THE ONLY PLACE YOU HAVE TO LIVE."
by Jim Rohn
"LIFE IS LIKE A VACATION AND YOUR HUMAN BODY IS THE ONLY PIECE OF LUGGAGE YOU HAVE WITH YOU AND THUS WE MUST TREAT IT WELL SO IT LASTS."
by Susan Peneguy
"IF THE FOOD DID NOT EXIST 100 YEARS AGO, DON'T EAT IT"
By Kevin Trudeau
"BE KIND TO YOUR BODY, IT'S THE ONLY ONE YOU GOT, MAKE IT LAST A LIFE TIME."
Found on a forum on a web page regarding alkaline diets.
"IF MAN MADE IT, DON'T EAT IT"
by Jack LaLane (age 92)
I think this is all very true.
I am neither a doctor nor a medical professional or a nutritionist and thus this is only my opinion. Yet I have read many nutrition books lately and I am now convinced that cancer (and other diseases) are the direct result of broken/damaged DNA (DNA is the blueprint for cells and found in every cell in our body). The human body is constantly making new cells and older cells deliberately die, are broken down and recycled. For example, red blood cells only survive about 120 days and white blood cells often last as little as a few days. Your skin cells last about 21 days. Villus Epithelium Cells in your digestive system last just 3-6 days. This is all very normal.
Thus our remarkable body is constantly making new cells to replace these now dead cells and breaking down these dead cells and recycling the parts when it can. Making a new cell generally means an existing cell splits into two parts (including the DNA) and now you have a new cell, complete with new DNA and so on. (The old cell has died and been recycled). But if a new cell has a defect in the new DNA (due to a transcription mistake, poor nutrition or a toxin in our body), that cell usually dies (known as Cell Apoptosis and often triggered by DNA gene p53) or the human body usually detects this DNA mistake and breaks down the cell since it is poorly constructed. It is said in one book that the human body beats off cancer cells 4 or 5 times over our life, before a defective cell can actually become a tumor.
To detect these defective cells and break them down, our bodies many complex parts must be working well together, i.e. our immune system, our lymphatic system, our circulatory system, our nervous system and so on. All our individual cells (we have 65-70 trillion of them in each of us) likely have a distinct life span, some measured in days and others in years. Each of these cells needs certain nutrients to behave properly. These nutrients include glucose (a form of sugar, obtained from carbohydrates in our diet), proteins (from meat and dairy products in our diet) and essential oils (ALA, DHA, EPA - from flax seed, olive oil and fish in our diet)). Glucose is the raw fuel each cell needs for life and the other materials (proteins, oils, minerals, vitamins, fats, etc) are building blocks for new cells etc. These building blocks are important for the proper functioning of your body (movement, speech, vision, etc) and proper cell construction - eat the wrong foods for too long and you will likely at least have poorly constructed cells or even worse. It is no surprise then that eating properly is very important. So how do we know we are eating properly?
Our remarkable and complex human bodies evolved over many thousands of years until we evolved to the state we are at now. Specifically, many thousands of years ago, man became an upright individual and commenced eating fruits, vegetables, fish and the occasional live animal he could capture and eat. Look at your teeth and compare them to the teeth of your dog or cat - our teeth are one hint that our bodies are largely designed by nature for fruits and vegetables while the teeth/fangs of a dog or cat tell you their bodies are largely designed by nature for meat.


Thus, our teeth are one (strong) hint that nature has designed us to eat fresh fruits and fresh vegetables.
One nasty disease is type 2 Diabetes. Glucose is the simple sugar that is the main source of energy for the body's cells. Your pancreas secretes insulin to help your body’s cells take in blood glucose and convert it to energy. If you have insulin resistance, your body's cells do not respond well to insulin. This form of Diabetes (type 2) is often the result of years of improper nutrition (excessive amounts of soda, snack foods, fast food, candy, refined food, fried food, etc) as well as obesity and inactivity.
In addition, did you know that cancer rates have been increasing since 1900? In 1900, Cancer was not even in the top 5 of Death Rates - now (2007) it is #1 (per USA Today, 8/24/2007, page 5A). Look at this table showing death rates in 1900 and 1998 (I wish I had 2006 data but I don't as yet):
1900 Top 5 Death rates 1998 Top 5 Death rates
11.8% Pneumonia 30.4% Heart Disease
11.3% Tuberculosis 23.0% Neoplasms (Cancer)
8.3% Diarrhea/enteritis 7.0% Stroke
8.0% Heart disease 5.3% Respiratory disease
6.2% Stroke 4.1% Accidents
(see also http://www.infoplease.com/ipa/A0922292.html
Here is another piece of data from Rockefeller University showing causes of death since 1900 (thru 2000). You can see that only Neoplastic (Cancer) has increased over time:

So what happened? I am not sure but I know the food industry tried to increase the shelf life of foods so they added partially hydrogenated oils and preservatives, starting in the 1950s or so.
These are NOT found in nature and thus certainly not good for us (the partially hydrogenated oils and preservatives). To make it taste better, the food industry also added many forms of sugar (fructose, sucrose, galactose, dextrose, splenda, maltose, etc) to sweeten it and thus enhance the taste. BUT WE SHOULD EAT WHAT IS GOOD FOR US AND NOT WHAT NECESSARILY TASTES GOOD. Taste is not an indicator of the quality of the food, in many cases.
I think we should stop eating sugar-laden food, refined food (like breakfast cereals, white bread, white rice), fast food, butter/margarines, candy, cake, frozen dinners/pizza, fortified breakfasts and so on. Avoid food that contain sugars, high fructose corn syrup, partially hydrogenated anything or artificial colors or flavors or preservatives or any chemicals. Any oils you consume should be liquids at room temperature (thus avoid butter and especially margarine). Avoid trans-fatty acids (like New York City is actively doing now). Avoid artificial sweeteners - in general - if the food item is made by man, why eat it (per Jack Lalane)? If this food item did not exist 100 years ago, why eat it now (per Kevin Trudeau)?
We also need to stop microwaving food as the microwaves target the water molecules in food and thus microwaves likely disrupt the nutrients that are in the food (Most nutrients are water-based). I use our microwave very rarely now, largely for heating water.
So we should switch to what our complex bodies need (and expect) and only then will our body’s complex biological systems get the raw materials they are designed for and thus need (to properly work). Generally speaking, eat natural fruits/vegetables in a wide rainbow of colors every day and skip the sodas, candy, cake, fast food, frozen pizzas, the TV dinners and so on. I was perhaps the worst offender of eating poorly and ended up with Cancer.
As a result, I have dramatically changed my diet since I started battling cancer (I now eat only raw and fresh fruits and vegetables and some pure juices (with no additives)). Every day I am eating fresh blueberries, blackberries, raspberries, strawberries, onions, cinnamon, oregano, pomegranate juice, flax seeds, prunes, kale, garlic, radishes, V8 and so on). The water I drink is very pure also (effectively rain water). I also take a multivitamin (includes selenium). I soon plan to add (wild, not farm raised) salmon to my diet to get the essential DHA and EPA oils. (EPA has natural anti-inflammatory properties. DHA serves as the primary structural lipid of the brain and retina of the eye). I also take fish oil gelcaps, l-lysine pills, curcumin gelcaps and Calcium Citrate pills every day. I also take Vitamin E (the d-alpha kind, NOT the dl-alpha) and Vitamin D-3 (Sunshine turns a cholesterol-like precursor in our skin into Vitamin D-3 also and 30 minutes of sunshine per day generates about 10,000 to 12,000 international units (IU) of Vitamin D-3). Vitamin D-3 is also known as cholecalciferol. Once you start eating properly, expect it to take a few weeks/months for your health and appearance to improve because cells in your body have a definite lifespan and only when the new cells are created will they take advantage of the changed/improved diet to use for the new cell construction.
I have been doing this for 3-4 months and I feel generally fine and my family and friends say I look the best I have in years (many people think I am 45 or younger –I am 56!). My message here is to skip sugar (cancer loves sugar), white bread/rice, butter, margarine, fast food (McDonalds, Wendy's, Pizza Hut, Burger King etc), frozen food, refined food, snacks, cake, candy, sodas and instead go for fruits and vegetables--take them home, wash them thoroughly and eat them. I mix all my fruits and vegetables in a blender and it works for me and it may work for you. When you shop for food, read the ingredients first to see what is in that food and avoid those that have coloring, preservatives or sweetening ingredients.
I should add I also make it a point to walk at least 1 ½ miles with my dog every day. I do this to get some needed exercise that also helps the body in a variety of ways. I think most people were more active until the television became widespread in the 1950s and then the computer in the 1980s. My point is we need to be more active, even if simply walking every day. It helps with digestion, muscle tone and so much more. After all, many thousands of years ago, nature designed us to walk upright and hunt or gather fruit and vegetables. We need to keep active as that is what are our bodies are designed (by nature) to do.
Ask your doctor or nutritionist if you have questions about this. I also welcome your comments on this topic.
By the way, the books I have read include Fantastic Voyage, Live Long Enough to Live Forever (highly recommended!) by Ray Kurzweil & Dr. Terry Grossman (2004), Beating Cancer With Nutrition by Dr. Patrick Quillan ND (2005), How to Prevent and Treat Cancer with Natural Medicine by Dr. Michael Murray ND (2002) and Dr Katz's Guide to Prostate Health, from Convention to Holistic Therapies by Dr. Aaron Katz MD, (2006).
Two excerpts from the books:


You can download a copy of this (in Microsoft Word format) by clicking here.
Back to top
7/12/2007-I spoke with a nutritionist by phone and she pointed out I am taking in a lot of sugar with the fruit drinks and asked me to avoid the juices which add about 1 ounce of sugar per 8 ounce glass(!). My fasting glucose level is 105, a bit high so I plan to get this checked again. Hmmmm....I plan to meet with a nutritionist soon on this and other matters (i.e. curcumin etc)
7/18/2007-I had an eye exam on Monday (for the 1st time in years!) and they said my eyesight is great and there are no sign of glaucoma or macular degeneration. They did say I should use sunglasses outside on sunny days (I am fair-skinned) and I am to keep using my reading glasses. The eye Doctor also said I do look quite healthy.
Yesterday I went to NYC to see my oncology team and first I had a blood test and then a meeting with my Medical Oncologist and he said the fatigue I am feeling is the result of the IMRT radiation (55 Grey Units) combined with 5 months of strong chemotherapy and also the difficulties I underwent last fall (numerous bladder problems resulting in 7 visits to the ER and numerous days in the Hospital and tremendous blood loss resulting in a long hospital stay). He said to walk more and more each day to rebuild stamina and hold off resuming work until we revisit this sometime in September. He also said to take Vitamin D3 and also suggested ginko biloba (an OTC herb alleged to help with memory). He also gave me another dose of zometa (strengthens bones)and said I will likely get this every 3 months. Regarding symptoms of chemo brain, he stopped Lupron because it may affect the brain and it is unlikely helping due to the nature of my cancer. My Radiation Oncologist then sat with me and asked re lingering symptoms and I said the main one now is fatigue and he concurred that radiation fatigue does linger for 4-6 weeks after it ends. We talked about my petscan of 7/3 and he said he would double-check it for me and called me last night to say it looked good.
Today I went for a routine dental visit and the receptionist said I look great and I also looked 10 years younger! My teeth are also doing well (no doubt due to my changed diet and more thorough care of the my teeth).
Tomorrow I see my internist for a fasting glucose and triglycerides test and perhaps a complete chemistry profile.
7/19/2007-I met with the family doctor and he took a number of blood samples to check my overall chemistry as well as Thyroid function, Hemoglobin A1C, (fasting) glucose levels, (fasting) triglyceride levels and also liver and kidney profiles. He said I look great, my skin looks good and also I am doing the right thing in battling cancer and he has never seen someone do it as well as I. He will have the blood test results on Monday for me.
Also according to my sister-on-law "I last saw Joe at Christmas time; he looked like he was on death's door. I just spent the weekend with him and my sister in Naples, FL-- he looks fantastic, healthier than ever. Whatever he is doing ... it is working"
7/25/2007-I went to the Dermatologist for an annual checkup. He said I look fantastic and my skin looks great. I told him it is likely my revised diet. I then went to my Internist to pickup the blood test results (see 7/19/2007) and he said overall my results are good and to resume Lopid but now just once per day (in the morning).
My fasting triglycerides had been 900-1100 5 years ago but now it is 300, all from my diet so seems to be helping here also. I faxed the blood results to NYC to my urologist and my medical oncologist. Tomorrow, I go to NYC to get an MRI of my brain as a petscan does not work for the brain. Basically, a petscan tracks where the body is using fuel (glucose, a form of sugar). Cancer loves sugar so the petscan finds cancer this way. But the human brain always wants glucose also so the petscan cannot see cancer in the brain and thus an MRI makes sense in this case.
7/26/2007-I went to NYC and had an MRI of my brain - it took 25 minutes in all and about 1/2 way through, they gave me an injection of a contrast to show the brain easier. The contrast is Gadolinium which provides greater contrast between normal tissue and abnormal tissue in the brain and body. After it is injected into a vein, Gadolinium accumulates in the abnormal tissue that may be affecting head. Gadolinium causes these abnormal areas to become very bright (enhanced) on the MRI. This makes it very easy to see. Gadolinium is then rapidly cleared from the body by the kidneys.
This MRI is not painful but it is confining and quite noisy. The noise comes from very strong magnetic fields being turned on and off. Now I await the results which I hope to get on 7/27/2007.
7/27/2007-The Radiologist report on the MRI of my brain is unremarkable - this means no sign of lesions, tumors etc. The petscan (7/3) also said the same for the rest of me. Thus, as of now, there is no sign of cancer in me. I am due for another round of tests every 3 months (cat scan/petscan, bone scan, MRI) for the foreseeable future and the doctor does think the cancer will likely come back in 2008 although some patients take longer to see the cancer again (a healthy lifestyle may preclude it from coming back). Below is the actual MRI radiology report:

8/5/2007-I met some strangers last week at an airport and they were shocked when I said was 56 years old. They all thought I was in my early 40s! Click here to see what I eat everyday which is likely resulting in me looking younger than my age.
8/13/2007-we went to a wedding in Vermont this past weekend (OBVIOUSLY my wife drove the 360 miles round trip). It was a lot of fun but by 930pm I was wiped out and we had to leave at that time both days. But people there were stunned when I told them I was battling cancer and hopefully winning as they say I looked very healthy (likely due to my diet and supplements). My friend S.Chawla offered in an email to me that "You looked f...ing great, and I mean that". I am back home now and trying to walk more and more each day to regain my stamina.
8/17/2007-I drove my son to the airport and then I drove home (90 miles) and it did not seem to bother me too much. I think my stamina is slowly coming back (I am 56 and not 26 so it will take a while). I will keep walking a few miles each day to continue rebuilding my stamina ... I do want to get back to work sometime next month.
8/20/2007-My sister thinks I look 40 years old (not 56!) This diet is really working - it just takes time. I stumbled upon a very good description of a cancer description. Click here to see it.
8/22/2007-I went to a wedding in Vermont and my good friend Phil snapped a photo of me. Compare this photo to the one of me on 11/25/2006 when I nearly died.

9/14/2007-I am still battling stamina issues. I walk in a hilly area some 2.2 miles every day but am wiped out by 7pm when I do that and often asleep by 930pm or so. But I will keep walking every day to rebuild my stamina. My medical team postponed me going back to work until sometime in October, largely due to stamina issues. I suppose this is no surprise as I went through 2 rounds of chemo (most patients only get 1 round) and I also had some 31 days of IMRT 3D radiation as well. Stay tuned.
9/24/2007-I helped my son install cabinets in our laundry room and this involved measuring, cutting, hammering and he did the bulk of it and yet I was still wiped out by 8pm - my wife kept saying to me - "go to bed - you are tired!". So I did and fell asleep by 930pm and slept until 830am today. I just hope my stamina comes back soon - I do walk some 2 miles every day just for exercise and I live in a hilly area so it is truly a work out. My next PetScan/Catscan is scheduled for 10/3 in NYC.
10/10/2007-On Sunday 9/30, I was sitting outside and noticed a strange dull pain in my back somewhat on the right side. Later in the day I did not feel well so I went to lay down and then became violently sick, vomiting up all the days food. I slept fitfully and woke up the next day feeling much better. I chalked it off to a 24 hour bug or something like it. But I later found out it was likely due to a blockage in my gall bladder(!)
On Wednesday 10/3, I went to NYC for a combined catscan/petscan and I received the radiology results a few days later. I also emailed my medical oncologist and mentioned the Sunday incident and he said my gall bladder showed up in the petscan with gallstones. So I may need to see a GastroIntestinal doctor and/or a surgeon to either remove the stones or the gallbladder. The gallbladder is essentially a storage bag for bile, created by the liver to dissolve fat. The Petscan also showed the area where I had radiation somewhat active apparently consistent with the radiation I received. You can see the 2-page radiology report below:


10/17/2007-I met with my medical oncologist yesterday and we discussed a number of things and then my wife mentioned I am having short term memory lapses (I guess that is true - I do not remember!). This is a well known phenomena known as Chemo Brain which is likely a direct result of all the potent drugs I have received (Lupron, Taxotere, Kytrile, Zometa, Cisplatin(!), Etoposide, Flomax, Zofran, Percocet, Oxycodine, Fentanol and many many more). My stamina is slowly getting better and I do try to walk 2+ miles every day with my dog, up and down the hills where I live.
The doctor said I am to stay home another 3 months due to “ChemoBrain” and Stamina issues and I am to work on these as best I can. I see him again in mid-January and will likely get another petscan at that time.
My doctor then arranged for me to receive a Zometa infusion (to help rebuild my bones which are quite weak in the left pelvic area-right now, I am not allowed to lift more than 25lbs for the rest of my life). Basically this is a 4mg dose of Zoledronic Acid mixed with 100ml of 5% dextrose and infused into me via an IV over 30 minutes. Then they gave me about 500ml of 5% Saline solution to flush out my system (normal for Zometa). I may get this drug every 3 months for a period of time.
I see another doctor on 10/23 regarding my gall bladder (gallstones and blockages) that may require (laproscopic) surgery. I did have an apparent gall bladder attack on 9/30 (see above).
10/18/2007-A nurse called me yesterday regarding my meeting on 10/23 and she asked a few questions about my health and she did say my chemotherapy (which I had plenty of) can cause gallstones(!). That reminded me of what my Internist told me some months ago namely that chemotherapy has resulted in some of his patients developing diabetes after the chemotherapy ended.
Anyway, I checked my earliest catscan (from 12/2005, well before any chemotherapy) and it shows calculi in my gall bladder - translation - gall stones. Gallstones tend to result from either too high a level of cholesterol (from your diet and liver) or too low a level of bile (from your liver). My diet before cancer was not good and this may well be why I have gallstones which I think are just crystallized cholesterol. I am very very careful with my diet now as we all should be as “None of the risk factors for cancer is probably more significant than diet and nutrition” per the document "Advances in Cancer Research Volume 32 (page 329)".
Next update scheduled for 10/23 after I meet with the doctor.
10/20/2007-I am adding something new to my daily diet. Basically, in the book Outsmart Your Cancer (by Tanya Pierce) in pages 199-218 (Chapter 14), she discusses how a doctor (Johanna Budwig) researched how the body worked and discovered that each of our body's trillion of cells make use of Omega-3 and Omega-6 Oils in our diet for the individual cellular membrane and assist in each cells uptake of Oxygen that we breathe, i.e. the Omega-3 and the Omega-6 Oils help the cells attract the Oxygen to each cell and the Oxygen is then readily used in the cell. Not all oils do this she discovered.
She then researched the best way to make these oils more bio-available to the cells and came up with Cottage cheese due to the sulphur-based compounds in it. She then found the richest cottage cheese is known as "Quark". The book (page 208) goes on to say the likely daily diet is 1/2 cup of Quark and 6 tablespoons of a very good flaxseed oil such as Barleans (rich in Omega 3 and Omega 6 oils). One puts these two items in a small blender, adds some fruit for flavoring and mixes it up thoroughly. Then it is recommended you eat 1/2 of it in the morning and 1/2 in the evening.
What happens is that these Omega Oils are then distributed throughout the body and assist in cellular absorption of oxygen. What is key to know is Cancer cells cannot handle oxygen and are said to die if they take it into the cancer cell (there is very very little cancer of the heart as the heart has ample Oxygen from the lungs). So the goal then is to encourage all of your cells, including cancer cells, to readily absorb Oxygen. The good cells are happy and the cancer cells are damaged and will soon die.
The book has many stories of people who have killed their cancer with this approach and also mentions Cliff Beckwith and his experience with this diet. I urge everyone to buy this book Outsmart Your Cancer and read it for yourselves. It is a great book and I am on day 2 of this diet.
10/23/2007-I met with the Surgeon today and he recommends Laparoscopic Gall Bladder Surgery (on 11/28/2007). This surgery is mildly invasive but I will still be under general anesthesia as they cut small holes in my upper abdomen, inflate my abdomen area and then remove my gall bladder (due to gall stones). It is said to run 1-2 hours in length and I will be able to go home sometime afterwards and then I am to take it easy for 5-10 days. I also spoke with their staff and they provided me these specific instructions:
* - I am to meet with the Pre-Admin team on 11/14/2007 where I will be given a fasting blood test, a urine test, an EKG and a Chest X-Ray. I will also consult with the Anesthesiologist to discuss any drugs I take as well as any history of complications with anesthesia.
* - I am to see my primary care doctor (11/26/12007) before surgery to clear me for surgery.
* - I am to cease taking many drugs about a week before the surgery date (11/28/2007): Aspirin, Ibuproften, NSAIDS (Motrin, Alleve, Advil etc), Vitamin E, Coumadin, Glucophage.
* - I will also cease eating tomatoes in any form in the week before. All this is largely to reduce the chance of bleeding during surgery.
* - In the evening before surgery, I am not to eat or drink past midnight.
We also met with my medical oncologist shortly thereafter and he strongly recommended I have the gall gladder removed, based on the radiology report from the pet scan of 10/3/2007. So it is now scheduled for 11/28/2007.
11/11/2007-not much is really new with me yet I did attend a dinner last Thursday with my wife and saw many long time friends. What struck me is a number of men there are also battling cancer and one of them may have the same cancer I do (my cancer is exceedingly rare!). I give them all my business card and asked they email me and I will direct them to this web page as well as send them some other tips, i.e. who my medical oncologist is etc. But it was striking to me to see 2-3 men there with prostate cancer and another with non-hodgkins lymphoma. So far I feel fine and no sign of cancer in me thus far but I am VERY careful what I eat (see above) and I hope that helps me. Right now I am slowly getting ready for my gall bladder surgery on 11/28. This means getting pain killers ready and finding antibacterial soap and so on. I see my family doctor on 11/26 to get the green light for my surgery and then call in the night before surgery to find out what time I need to be there. Stay tuned.
11/26/2007-My family doctor examined me and said I was ready for surgery. The examination included review of blood tests etc.
11/28/2007-Today my gall bladder is scheduled to come out and we had to be at the hospital by 545am as surgery was 7am.
12/5/2007-My gall bladder was removed laparascopically a week ago today and the surgery was amazing and uneventful. It required they insert a camera, lights and CO2 gas into my abdomen and then insert surgical tools to cut the gall bladder loose and then remove it (via a surgical incision in my belly button). I was under general anesthesia the whole time and surgery lasted just under 2 hours and I went home later that day. I was in pain for about 48 hours or so afterwards and they advised me to not lift anything heavy for at least another week. I have three very small incisions in my abdomen as a result of this surgery.
12/15/2007-I am largely recovered from the surgery and I notice no change in my eating habits. It is said the liver will compensate to some degree when the gall bladder is removed, i.e. it builds a much smaller gall bladder to hold the bile that the liver makes. (Bile is used to dissolve any fat in the food I eat).
01/05/2008-I am scheduled for my next PETSCAN this coming Monday at 10am in NYC. I have noticed no side effects at all from not having a gall bladder. I still get tired a little easy and I do notice memory lapses (chemobrain).
01/08/2008-The latest petscan (1/7) results shows NO sign of cancer in me despite the fact that it kills 98% of those who contract this form of cancer. I think my radically changed diet is keeping it from coming back (my heroic doctors in NYC did knock it down some months ago with intense Chemo, followed by IMRT radiation). I will post the radiology report itself in about a week.
01/15/2008-I met with my Oncologist today and he was happy to hear there is still no sign of cancer in me. (I must be "strong in all the broken places"). He said the next goal is to go another year without any sign of it. I asked re blood tests to catch signs of cancer before a petscan might show it and he say probably not worth it as it would not change his approach to battling this cancer. He said if it does come back, he will likely use the same chemo approach. I then met with the surgeon who did the gallbladder removal and he said I healed very well from his incisions. I also received another IV Infustion of 4mg Zometa (in a 5% Dextrose 100ml solution) over 30 minutes to help rebuild my bones.
02/18/2008-I went to my dentist for a regular visit and my mouth continues to improve, no sign of inflammation and all looks well. They were quite pleased and this is in stark contrast to Sept 2006 when I was about to undergo dental surgery to repair heavily damaged gums (periodontal disease) and suffered routine bleeding of my gums.
I still suffer from stamina issues so I now walk on my treadmill every day to help build it up again but my impaired blood counts also could explain the stamina issues.
My SO scheduled a visit for me with a Neurologist to assess my lingering memory problems. I told I her I do not recall any memory problems (!). I see this doctor in early March.
3/10/2008-I met with a Neurologist (on 3/3/08) and he asked me many probing questions and then said I appear fine mentally, i.e. typical for someone my age. But then he read emails that were sent to my wife (which we brought with us) and said I should likely be at the 90% percentile and not a typical person so to speak. So he suggested more (mental) testing at NYU. He also said there is no sign of Alzheimer's in me.
I also met with my family doctor (3/6) and he said I look fine and he took many blood tests (lipid profile, sed rates, a1c, thyroid, CBC etc) and I should have the results back soon.
3/29/2008-I am having another petscan on 4/9 and then a meeting with Oncologist on 4/15 and then more testing at NYU (10am-3pm) 4/29, 4/30 and 5/1. Otherwise I feel generally fine. My 3/6 blood tests came back and RBC and WBC remain low. My C-Reactive Protein was 0.5 and my Sed rate was also low at 1.0. My fasting glucose level is 85. My cholesterol was 201 and triglyercide number is 157 (this is high but was 1100 at one time and I reduced it through diet and exercise).
4/10/2008-The latest petscan results are back and to quote my oncologist "No evidence of relapse. overall OK". That is terrific news considering only 2% of people survive this cancer (and median survival time is 2-7 months). I see my oncologist on 4/15 and then more tests at NYU at the end of the month.
4/15/2008-We met with my Oncologist (Dr DavidN) and he said the petscan looked good and did say they spotted two areas (near the lymph glands at the top of lungs) that lit up somewhat. They were symmetrical so they do not know what it is. He felt it could be inflammation or something else. He asked I get a petscan in 2 months (without a cat scan this time) to see if it changes at all. He also said to see him in 3 months for my normal appointment. Regarding my Zometa infusions (which I have received every 3 months, including today), he said to get them every 6 months now so the next one is around October 15th.
He also said if I go 2 years it is possible I am cured and if I go 5 years, then I am cured. This is all measured from the date of last chemo (2/8/2007). I asked re RBC and WBC counts remaining low, he said that is due to chemo/radiation and he did not see the need to use drugs to boost them, at this time. I also asked him for a nutritionist reference and he concurred. I asked to be sure I am eating properly (too much complex carbs perhaps?).
5/7/2008-Well much has happened - I spent 3 days going through some thorough neuropsychological testing at the recommendation of my neurologist (this testing was held at the NYU Medical center in NYC). My brain actually hurt at end of day 3 as there were many intense tests. The NYU doctor said my stamina problems are known as neurofatigue, i.e. my brain gets tired compensating for deficiencies in certain mental processes. Anyway, as a result of all these tests, they determined I am both mildly and severely impaired in some ways (as a result of intense chemotherapy) with some mental processes. I will have the details on the nature of my impairment next week.
I personally do not notice these deficiencies myself but many others (family, friends) have told me I repeat myself often, have short term memory lapses and have some concentration issues, all a result of many chemo drugs I received (etoposide, cisplatin, taxotere, lupron, etc). Hey - at least I am alive (my form of cancer kills 98% of men who get it) and I am apparently healthy.
5/22/2008-I finally received the medical report from the NYU medical center and I have been diagnosed with encephalopathy. A more common name is Chemobrain or chemofog. This means my brain has been impacted by all the potent drugs I received in this battle with cancer. Apparently I have problems measuring time, multitasking, prioritizing and I suffer from short term memory lapses. These effects may well be permanent also. At least I am alive and I would rather beat cancer with some mental impairments as opposed to cancer beat me (kill me) and have no mental impairments. At least I can talk to people, read books and so on. More details on chemobrain can be found here.
06/12/2008-Nothing really new but I have resorted to writing lists due to short term memory problems and I find I start projects at home and rarely finish them - all likely due to chemobrain. Oh well. The next step is another petscan on Monday (6/16) and this will be solely a petscan (without the usual catscan for calibration) and nothing else as they wish to see if there any changes in the hilal area of my lungs which were lighting up on the last petscan (lighting up means absorbing glucose which cancer also does). Doctors do not seem too concerned as it is lighting up in both lungs in the same place (bilaterally) so inflammation is more likely. Stay tuned.
06/17/2008-The latest petscan results still show no sign of cancer and the inflammation spotted last time (4/15) is greatly reduced. I did look at the images and I did see a suspicious spot near my bladder. I am not a doctor so I printed it off and showed it to my oncologist and he said not to worry yet and he will talk to the doctor who studied them and also bring it up on Monday at the weekly meeting where they discuss all patients. He asked me to email him on Tuesday 6/24 for the results of what he finds. If it is cancer coming back, it is quite small but my sense is it is not cancer. Stay tuned.

7/8/2008-The radiologist confirmed the spot is not cancer but FDG ( fluorodeoxyglucose) moving from my kidney to the bladder. FDG is used during petscan imaging. Hoorah!! I still suffer from ChemoBrain though and next petscan will be in September and then again December and then next year will be every 4 months and not every 3 months.
7/29/2008-Nothing really new - I may be applying to the Kessler Institute for ways to compensate for encephalopathy. Otherwise, I am doing fine.
8/1/2008-Yesterday, I met with my dermatologist for my annual checkup and he said my skin looks great and may well last another 100 years. I then had my first meeting with a psychiatrist, just to explore issues. I see him again next week and not sure beyond that.
08/19/2008-My friend Phil came down and he and I reorganized some things around the house. I cannot lift more than 25lbs so he was very helpful on the heavier loads. I ended up walking (Saturday) some 23,000 steps (as measured on my pedometer), the most I had done in perhaps 5-8 years. My left hip (previously damaged by cancer) hurt a bit so I took it easy on Sunday and it feels fine now. I remain very cautious on what I eat and continue the Johanna Budwig diet as a way to keep cancer from coming back. I also consume some 20-22 supplements per day as a method to keeping me healthy.
Per a good friend of mine:
Your spirit is incredible. I have read your blog from time to time and can not begin to imagine what you have had to endure. One challenge after the next and you meet every challenge with seemingly good spirit and great dignity - a role model for all of us.
9/11/2008-I had another petscan today and took the disc home and examined my images and still no sign of cancer from my viewing of the images. This is in spite of the fact my form of prostate cancer kills 99.9% of people. My diet is certainly helping.
09/12/2008-I received the radiologist's medical view of the petscan from yesterday and the doctor's report said no sign of cancer was found. Hoorah!
09/17/2008-I met with my medical oncologist yesterday and he said "you are doing AMAZINGLY well" and said I will keep getting petscans every 3 months until the 2 year anniversary of last chemo so after 2/9, I will get them every 4 months. He also looked me over, used his stethoscope etc and said I am doing fine.
10/6/2008-Met with family doctor as a routine checkup and he did extensive blood tests as well as a urine test.
10/10/2008-The blood test results shows my RBC remains somewhat low and this is probably for life as cancer destroyed part of my left hip where blood cells are often made. A low RBC means I get tired easily and am perhaps out of breathe faster than the typical person.
11/25/2008-Insomnia remains a real issue with me. Tylenol PM does help somewhat. Otherwise, I am generally okay, ready for the next pet scan (12/16/2008).
12/18/2008-I had a full body petscan (head to toe) on 12/16/2008 and still no sign of cancer. I met with my onocologist today and he says petscans now every 6 months for 5 years and then once per year thereafter. He was quite happy that I am beating this cancer and attributed it to luck. I respectfully disagree-these three steps likely significantly helped as well:
1-I adopted the Johanna Budwig diet
2-I avoid all man-made (processed/refined) food as much as possible
3-I embrace fruits and vegetables as much as possible.
FYI: I also received another 4mg Zometa infusion today.
03/23/2009-Next petscan is a week from today (3/31/2009) and I am getting them once every 4 months now. I see my oncologist on 4/2/2009- stay tuned. My insomnia is largely gone- likely due to 1000mg of Tryptophan every evening. I think the daily 30mg of Abilify was causing the insomnia.
04/02/2009-The petscan showed a small metabolically active tumor (1.9cm x 1.6cm; about the size of penny) near the right anterior abdominal wall, about 5" below my belly button. It was also seen in December and was just 4mm then so it has increased in size by 16fold and is now hypermetabolic (it was not metabolically active in December which is why it was not noticed then).
We met with my medical oncologist and he said a biopsy is in order and they will also meet on me as to next steps (chemo, Surgery etc). Oh well...I will know more next week after that meeting among the doctors. My doctor said he was unhappy it came back but that it usually does within 2-3 years. Stay tuned. Oh well, I was in remission for 2 years, 1 month and 10 days (771 days in all).
04/11/2009-They looked inside bladder (4/10) and said there is no sign of cancer in there. It was a painless procedure. The next test is an endo-rectal MRI of my pelvic area and then likely meet with my oncologist as to next steps. Stay tuned for results of the MRI.
05/06/2009-The MRI (4/24) showed no other signs of cancer and then I had a biopsy (4/28) of the new cancer and they called it adenocarcinoma. I meet with my medical oncologist on 5/12 as to the next steps. Stay tuned.
05/13/2009-I met with my medical oncologist yesterday and he said no chemo (too toxic) but was open to using casodex and antibodies to go after it. The oncologist also said regular petscans will be used to continue to monitor me for new cancers since the petscan of 3/31 found this one. He was agreeable to surgically removing it so he referred me to my urologist who will do the surgery. Then I commenced the pre-surgery process, i.e. got an EKG, some blood tests (5 in all), filled out many forms and so on. They also told me to stop all medications and supplements a week before surgery. After all this, I received my regular zometa infusion. It was a long day in NYC. I also need to be cleared by my internist for surgery also and that will happen in the next few days. Surgery itself will be on Tuesday June 9th.
05/29/2009-I met with my internist on 5/26/2009 as he has to clear me for my upcoming surgery. He said I am able to tolerate surgery so now I wait until 6/9. I plan to stop all supplements on 6/1 (some 22 in all, including Vitamin E and 81mg Aspirin) as preparation for surgery.
06/15/2009-
 (photo is from my wife's cell phone and shows my son and I right after surgery).
(photo is from my wife's cell phone and shows my son and I right after surgery).Surgery was in the evening of 6/9 and lasted 90 minutes or so. I was in my room by 10pm. I was put on Fentanyl as a pain killer, via an epidural (4cc/hr). I was on a clear liquids diet until my digestion system 'woke up' which was on Thursday (passing gas or a bowel movement was the signal they looked for) so I switched to a regular diet Thursday evening. The Foley catheter came out on Wednesday evening. I was on 2x daily colace to keep stool soft to avoid straining which could be a BIG problem right after surgery. Dr EDV and his assistant KathyH also stopped by to check on me on Wednesday and other Doctors from various specialties (urology, pain management, anesthesiology) came by every day to check on me. They removed the epidural on Thursday and switched me to Percocet (2 tablets every 4 hours). The hospital itself also sent numerous people to see me (a welcome person, a concierge person, a person who checked on my room, a lending library person etc). The doctors had me walking every day and I came home on 6/12. I notice I am getting better every day in terms of the surgery but it will still take some weeks before I am back to normal. I remain on one colace daily and one percocet every 6 hours.
06/23/09-I met with my Dr EDV, my urologist (he did the surgery) and he said the incision looks good and I am allowed to drive, go swimming etc but do not lift anything heavy for 4 more weeks. He also said I do not need to see him again for this. He also said the surgery was uneventful, i.e. no hives or any other issue. I then met with my medical oncologist (Dr DMN) and he said pathology showed different types of cancers, some hormone sensitive and some not. Specifically, one of the types of cancer was acting like small cell cancer. He then indicated it is time for another petscan (within the next 2 weeks) and then I am to commence casodex after that and also see him in 4 weeks. He also said he may put me on a milder form of chemo also. In closing, they will also study the tumor they took out of me.
06/30/09-The petscan is now scheduled for 1230pm on 7/8; no food to be eaten past 830am. Theoretically, if no cancer is spotted, I commence a casodex (Rx) regimen and petscans will continue every 3 months. If cancer is detected, I commence chemotherapy. It is felt the cancer they removed on 6/9 came from one cancer cell that did not get destroyed during prior chemo and radiation and thus grew in size until detected in the petscan of 3/31 (see above). The next doctor (medical oncologist) appointment is Dr DMN for 7/23 at 11am and we will discuss the petscan and next steps at that time with Dr DMN.
07/09/09-The petscan was 1230pm yesterday and was a full body scan. It showed some spots that were mildly hypermetabolic so a bone scan is scheduled for Monday. Dr DMN (in an email) said the petscan was overall good so he likely just wants to rule out cancer where it showed mildly active or else get a better picture of it. The Bone Scan is set for 7/13 @ 11am.
07/13/09-I had a bone scan today...basically, they inject Technicium 99 (a radioactive isotope) that is attached to phosphorous into me. The phosphorous is attracted to the bone so it lights up the bones for the scan. After they inject you, you need to wait 2 hours for it to work. Then you lay down and a machine moves over you slowly, taking 30 minutes to fully image you. So the whole process was close to 3 hours (including filling out forms, waiting etc). I will likely have the results tomorrow so stay tuned.
07/19/2009-The bone scan confirmed two spots had cancer-one near my left shoulder and the other on the 4th bone from the bottom of my backbone. I see my medical oncologist on 7/23 and will get his treatment approach at that meeting.

07/23/2009-We met with the medical oncologist and he wanted some blood for a special study (a research project that detects "circulating tumor cells in prostate cancer") which I agreed to and then we talked about what to do next. The study results will come back early next week so we opted for 30 days of Casodex (an anti-androgen drug) and then will meet again (in 30 days) and we will then discuss commencing with chemo drugs, depending on the study results. The Casodex I am using is the generic version and I commenced on 7/25/2009.
07/28/2009-I met with my medical oncologist today as he wanted me in another research study. This one is called "Molecular Basis of NeuroEndocrine Prostate Cancer" - I am one of 40 people in this study and my doctor is leading this study effort. They also took 3 vials of blood for this study to study the DNA and RNA from my white blood cells and compare them to the DNA/RNA of the tumor excised on 6/9/09.
07/31/2009-The Ciruclating Tumor Cell research study came back as 1. This is good news in that the doctor had told me anything below 5 is good. He had cautioned this test is imprecise but at least I am on the low end.
08/27/2009-We met with the oncologist and he said that the results of today's PSA test will tell him what to do next. He also said the casodex I am taking is keeping it from growing and that the tumor expresses PSMA (prostate-specific-membrane-antigen). He said a bone scan is to be scheduled the next time I see him (9/22-11am). He also scheduled me for a Zometa infusion on 9/1 (11am). I asked him about seeing Dr A. Katz and he felt it could not hurt and may help.
I also saw a Retina specialist today to look at my right eye which shows lattice in it. He felt it was not a problem and to keep getting eye exams every year and to call him if my eyesight worsens. Overall, he said my eyes were fine.
9/2/2009-I went into NYC yesterday to get another dose of Zometa and also pick up the blood chemistry reports. I found out my PSA dropped from 1.85 on 7/23 to 0.42 on 8/27 so I guess the casodex I am taking is working.
9/24/2009-We met with the Oncologist on Tuesday (9/22) and he said the very preliminary results from the study on my abdominal tumor was that it was a fairly unique tumor in terms of its genetic makeup. He then said to wait until the next bonescan (10/6) and petscan (10/7) and then we will talk (on 10/13) about the next steps. Meanwhile, I take casodex every day. Casodex shuts down the adrenal glands from making testosterone.
10/12/2009-I had a bone scan on 10/6 and a petscan on 10/7 and the results show the cancer is slowly growing in size in my left shoulder and less clear on growth in my l4 vertebrae. My left shoulder now hurts - did I sleep on it awkwardly or is cancer causing this pain? I see the oncologist tomorrow and we will discuss all these issues and more. The scans also shows some cancer in/near my left lung and my inferior right ischium (right pelvic region). So I have four sites with cancer. Stay tuned.
10/13/2009-We met with the oncologist today and he felt that more chemo is the best choice now (I had been cancer free for over 2 years) so I resume cisplatin and etoposide on Tuesday 10/20. He also said to stop the casodex as it is not helping. He ordered zofram for me and said to drink a lot of water on 10/19 and also thereafter. This is to flush my kidneys. Chemo is not easy as it really hammers the body....oh well.
10/21/2009-Today was day 2 (of 3) of my chemo regimen which goes in this sequence
1-they check my blood pressure, my pulse and my body temperature
2-They hook up an IV so they can infuse the drugs
3-They give me a (oral) pill (EMEND, 80mg) to stop nausea
4-They give me 1000 ml of saline solution through the IV to exercise the kidneys
5-The give me 16mg of Zofran (in 500 ml of dextrose) and also 2mg of a steroid drug (Dexamethasone). Zofran is a potent anti-nausea drug and works well for me.
6-They give me 182 mg of ETOPOSIDE in 500ml of dextrose and infuse that over 90 minutes
7-They then give me 79 mg of CISPLATIN in 250ml of a saline solution and infuse that over 60 minutes.
They also tell you to drink plenty of water when you get home as CISPLATIN can damage the kidneys if it is not diluted with water.
Each day is the generally same in terms of the regimen and tomorrow (10/22) is day 3 and the last day of this round of chemo. It is spread over three days as it is too toxic to be given in one day. The next round of chemo is likely 11/10 and will be given over 3 days again. I get 4 rounds in all of this chemo, each 3 days in duration.
10/22/2009-Today was day 3 (of 3) of my chemo regimen which goes in this sequence for today
1-they check my blood pressure, my pulse and my body temperature
2-They hook up an IV so they can infuse the drugs
3-They give me a (oral) pill (EMEND, 80mg) to stop nausea
4-The give me 16mg of Zofran (in 500 ml of dextrose) and also 2mg of a steroid drug (Dexamethasone). Zofran is a potent anti-nausea drug and works well for me.
5-They give me 182 mg of ETOPOSIDE in 500ml of dextrose and infuse that over 90 minutes
This day was different in that I did not receive 1000ml of saline nor the CISPLATIN. ETOPOSIDE is spread over three days as it is too toxic to be given in one day. The next round of chemo is likely 11/10 and will be given over 3 days again. I get 4 rounds in all of this chemo, each 3 days in duration.
10/26/2009-Chemo was last Tuesday-Thursday (10/20-22) and then my wife gave me a 6mg shot of neulasta (10/23) to help rebuild my white cell blood count as chemo destroys white blood cells. On 10/24, I had severe diarrhea from the chemo and my insides were gurgling like crazy. Yesterday, I started feeling noticeably better and today thus far I feel back to normal. The pain in my left shoulder is also greatly reduced. I see my oncologist tomorrow to discuss next steps, i.e. when do I get more chemo. He will also look at my blood chemistry tomorrow to see how I handled the chemo from last week.
10/27/2009-We met with the oncologist and he said the next round of chemo is 11/10-12 and I will also get zometa on 11/12. We asked about me being able to travel and he said it depends on my platelet count. It dropped from 228 to 162 in a week due to chemo-162 is still in the normal range but lower. He ordered a blood test for next week to see how my blood chemistry continues to change, i.e. does it get better or worse. He also felt it wise I get a flu shot and my wife also.
10/30/2009-I looked over my medical insurance claims and found out that
A combined Petscan/catscan costs some $5550
An MRI costs $3280
A bone scan xray costs $1135
Chemotherapy costs $1195 per day.
Otherwise I feel fine although I did get sick last night for no apparent reason. Weird.
11/5/2009-I notice my hair is starting to fall out, i.e. when I comb it, there is hair on the comb; I can also pull it out easily. This is no doubt due to the chemo drugs I received (10/20-22). The next round of chemo is next week, i.e. 11/10-12. I feel fine overall.
11/10/2009-Day 1 of the 2nd round of chemo commenced today. It was identical to 10/21/09 (above) except I was also given a seasonal flu shot (not H1N1) today. I plan to take a zofran pill around 10pm tonight so I am not nauseous overnight. Stay tuned.
11/12/2009-Day 3 was just like the last day 3 (see 10/22/09) except I also received Zometa today. This was planned...My stomach feels queasy from all the drugs so I will live on Zofran pills to keep it under control. I predict I will feel relatively normal again around Tuesday (Today is Thursday).
11/15/2009-Zofran prevents nausea very well but side effects from it are severe constipation so I had to radically change my diet to ramp up on fiber and also take Colace to ease the constipation. I also stopped taking Zofran after yesterday morning to help the process and luckily the nausea has subsided. I also should note my wife gave me another shot of neulasta on 11/13, to boost my white blood cell count. A low white blood cell count comes from the chemo and is dangerous as you can get sick easily with a low white blood cell count. The WBC cells help fight infection and thus you need to have a proper WBC count.
11/18/2009-I finally feel normal again, i.e. no queasiness in my stomach. I stopped taking Zofran on the morning of 11/14/2009,partially due to side effects and partially as I did not need it anymore. I have lost most of my hair as a result of the chemo drugs but I feel the chemo is working - pain in my left shoulder (from cancer) is gone. Let's hope the chemo works. Next round is likely on 12/1-3.
11/22/2009-I had a chest x-ray on Thursday to see is that cancer nodule in my lung has regressed. Per my doctor, the x-ray showed no nodules at all. This chemo must be working!
11/24/2009-I developed blisters on my left scalp and left ear. My oncologist thinks it is side effects from the chemo. They do not itch but I can feel them on my head.
11/25/2009-We went to NYC to see my oncologist and said I had shingles - UGH! We then went to an opthamologist to rule out shingles in my eyes. I am now on Valtrex for the shingles, 3 pills/day and my chemo has been cancelled.
11/30/2009-I went to the ER on Friday and they promptly admitted me for 4 days and 3 nights (at a total cost of $20,684.05) I was in isolation largely due to shingles (and a bad cough). They gave me high doses (via an IV) of antiviral drugs and antibiotics, every 6 hours or so. I am home now and shingles are still with me but fading away and I still have that cough due to post nasal drip. I will take it easy for a few days now and continue on antiviral and antibiotics (in pill form). Below is a photo of my head with shingles-UGH!

12/04/2009-The town sponsored an H1N1 flu shot clinic so I went to it and received a flu shot for swine flu (aka H1N1) today
12/09/2009-Chemo has finally resumed and today is day 2 (of 3) of round 3 of chemo. Tomorrow completes this round and then I get a petscan on 12/17/09 to assess the results of 1st 3 rounds of chemo (of 4). Stay tuned.
12/17/2009-I received a Zometa infusion today.
12/21/2009-The petscan is encouraging...some cancers are inactive (dead) and two others are shrinking in size. Round 4 of chemo is 12/29-31 and that is it for chemo for now. Let's hope it kills all the cancers. I still suffer from remnants of shingles-UGH.
1/5/2010-The side effects of the most recent chemo (12/29-12/31) were tough....I felt queasy through 1/3/2010 and got sick two times (at night, 1/1 and 1/2). Yesterday I felt remarkably better so I am past the chemo side effects. The side effects included destroying my GI tract temporarily. That came back to life on 1/4. Shingles are largely behind me now also-the searing pains are gone, thank heavens, likely due to a 200mg dose 2x daily of Carbamazephine (also known as Tegretol).
1/10/2010-The next step is likely targeted therapy for those cancer cells expressing PSMA which my cancer cells apparently express, per earlier lab test results. We did meet with the oncologist on 1/7 and he said to come back in a month and we will further discuss these next steps and also schedule a petscan now that chemo is done. I also see a neurologist in about a week to discuss shingles.
2/12/2010-I met with the neurologist 1/19/2010 and he said to stay on tegretol (2x/day) for a few weeks more yet and then cut back to once daily for a week and then stop altogether. I met with the oncologist on 2/9 and he said to schedule a petscan in 2 weeks (2/23) and he also gave me a brief physical, i.e. used his stethoscope and listened to me breath and also checked me for swelling in my extremeties (edema) and they also revieed my current medical history. We told him I am going for a hearing test on 2/15/2010 as I have trouble on the phone, especially cell phones. I usually have trouble comprehending the caller. This is a known side effect of certain chemo drugs (cisplatin). If the hearing test goes well, then it may be cognitive processing of the talking is impaired but it only happens on the phone so who knows? Anyway, I get a hearing test in 2/15/2010.
02/15/2010-I had a hearing test today and there was no change in hearing. We were concerned as I have trouble hearing on the phone. They did find a lot of wax (genetic basis) so they cleaned that out prior to the hearing test. The next item is a petscan on 2/23/2010.
02/26/2010-I had a petscan on 2/23/2010 and the results show all cancers are gone except for one on L4 vertebrae (in my spine). I hope to see the doctor on 3/2/2010 to discuss the next steps.
3/3/2010-I met with the oncologist yesterday and he said the petscan looked rather good and agreed that there is still some cancer remaining (only on the L4 Vertebrae). He offered radiation might work on that one spot but recommended a wait and see approach unless I feel pain from it. The cancer is too limited for the targeted therapy approach at this time. I will get another petscan in late May and we will discuss again when we meet on 6/8. So for now I watch for unusual pains as we wait until the next petscan.
3/12/2010-On Tuesday night (3/9), the big toe on my left foot (this happened about 6 weeks earlier when part of that toenail came off) started bleeding a lot from the right side of the toenail. We bandaged it up and I went to see a podiatrist on 3/11. He said my left foot's toenail would not get better as-is as he diagnosed granuloma - basically part of the toenail on the big toe was now below the skin line and my body's immune system was now mounting an attack on that part of the toenail.
The solution (painless) was to cut off that part of the toenail that was below the skin line and also cut away any dead skin adjacent to the toenail. He did this and then bandaged me up and said I can resume normal activities and to soak the toe in epsom salt solution (for 15 minutes) every day for 7 days. He also said my recent Chemotherapy might have caused this. He also said no need to see him again unless it acts up again. Never a dull moment in my life.
04/26/2010-I had my regular colonoscopy today and the doctor said it was very boring, no problems at all and I am to get my next one in 5 years. The cost was approximately $4800
05/18/2010-I had a petscan yesterday and it found cancer in 4 spots again - UGH! One on each hip, one in my spine (not new) and perhaps some in lymph glands. I see the doctor on 5/20 and will let you know what he says.
05/20/2010-We met with the Oncologist today and he said Provenge probably would not help me and he instead offered a Targeted Monoclonal Antibody Therapy that uses LU-J591 (an antibody protein that seeks out cells that express PSMA - which my cancer cells do - they attach a radioactive isotope to the protein and it kills the cells expressing PSMA via radiation. The isotope has a half life of one week.)
I may be a candidate for this therapy (depends on my blood chemistry and the type of cancer I have) and if so, I get an infusion of LU-J591 and then a bone scan a week later to confirm it is working and then another infusion. Only 52 patients are offered this therapy and I hope I am one of them. I had an EKG today and they took more blood for analysis all as part of getting into this therapy and also a urine sample.
If this fails or I don't get into this therapy, I am likely back on Chemotherapy, per the doctor-stay tuned....
I also signed up for a Circulating Tumor Cell study today wherein they analyze my blood to see if cancer cells are circulating in it and if so, what kind of cancer is it. Only 100 people worldwide are in this study. They took blood for this also. This will not help me but may help someone else.
05/26/2010-Met with the oncologist yesterday and they drew more blood for testing, i.e. what is my testosterone level as well as CBC and other tests. Then we talked about lowering my testosterone level with Lupron and Casodex. Lupron stops testosterone from being made (it shuts down the signal from the brain) and casodex prevents the body from using it. Lupron can cause bone pain until casodex kicks in. We agreed to hold off on Lupron until we see the testosterone level-lupron has side effects (affects memory). He gave me a Rx for casodex so I can move on that quickly once they know. They will call me today on what to do. I asked the doctor how fast Lupron works i.e. 2-3 weeks and he concurred with that. I asked if that would get me in the LU-J591 therapy but he was leaving the office by then and I didn't get an answer.
The circulating tumor study results came back. 0=best, 1-5 is good and >5 is bad. Mine came in at a 2 so it is pretty good per the oncologist. We talked about my PSA which is 3.3 - a little high.
After all this, I also received an infusion of 4mg of Zometa and then went home. I will likely see them next week, possibly for an infusion of Lupron- a single dose should do it. We want to lower the testosterone level as that is a precondition of the LU-J591 monoclonal antibody therapy.
Update#1: The testosterone came in low at 104. The nominal range is 175-781. Is that low enough? I emailed the doctor with the 104 level and asked if this is low enough for the LU-J591 targeted therapy or do I need Lupron/Casodex anyway to lower it further? I await his reply (via email).
Update#2: The doctor replied and said to commence with 50mg of Casodex (today) and I will get Lupron next week on 6/3 at 11am. I guess I need to lower my testosterone down to near 0 for the LU-J591 targeted therapy program.
06/03/2010-I received an injection of 7.5mg of Lupron which lasts until 7/1. I may get 22.5mg then (a 3 month dose). I then met my brother-in-law for lunch - he has prostate cancer also and was operated by robotic surgery some 2 months ago or so. He was back for a follow-up and it was serendipitous we both were at the same location on the same day and time. He lives outside Ithaca, NY and I live in northwest NJ.
07/06/2010-I just read Suzanne somer's book "Knockout" and learned many important things from the book:
1-The Budwig diet includes SIX tablespoons of flax seed oil mixed with 8 ounces of Quark - I had been doing 2 tablespoons and that simply was not enough. I divide it into two doses also. See page 216 of the book for details.
2-Green tea has something called EGCG (Epigallocatechin-3-Gallate) and studies (in mice with stomach cancer) show that ECGC shrank the tumors by 60% and the concentration of blood vessels feeding the tumor by 38%. See page 261 of the book for more details
So now I eat 6 tablespoons of flax seed oil in my quark and I also drink some 6 cups of green tea every day. Let's hope it works.
I see the oncologist on 7/8/2010 - stay tuned.
07/08/2010-I met with the oncologist and they took 5 vials of blood (CBC, CMP and three other vials). He said they need to see if my PSA is rising or falling-if falling, that is good (falling due to lack of testosterone) and then wait for a petscan (on 7/29/10). If PSA is rising still, I will likely go into the drug therapy program as my testosterone levels are likely quite low due to lupron on 6/3. The drug therapy program is LU-J591 (see 5/20/2010 above). I also received a one month dose (7mg) of Lupron again to keep testosterone levels low. I see the doctor again on 8/3/2010.
07/10/2010-My blood tests came back from 7/8 and my Testosterone came in at 16 (normal is 175-781) so lupron is working. PSA came in at 0.36, up slightly from last reading of 0.22
07/13/2010-I was walking our dog Sunday night and the rope became entangled in my feet just as the dog pulled so I went down in a very rocky area. I was cut in many places and bleeding from my right shin and I severely cut my left ring finger. My neighbor is on the local ambulance team and she looked me over and bandaged me up and said I should go to the emergency room. So we did that and they gave me a tetanus shot, an RX for antibiotics and then a nurse practitioner cleaned my wound on the left ring finger and then put 10 stitches in there (after first numbing the area). I was also x-rayed (my left hand and right shin) but no problems were found. We got home around 230am from the hospital. The medical people told me to remove the bandage from my ring finger in 24-48 hours - I will do that tonight. They also referred me to my family doctor in 10-14 days to remove the stitches.
07/30/2010-I had the stitches removed and my finger is getting better. I had a petscan yesterday and it showed just one site with cancer and that cancer is shrinking. The prior petscan (5/2010) showed 4 sites with cancer. So this is very good news and I will keep on my flaxseed oil/quark cheese diet regimen as I think that is why my cancer is receding.
08/03/2010-We met with the Oncologist and he felt the lupron was beating the cancer while I said I think the flax seed oil/quark combo is doing it. He said to keep doing it as it will not hurt and could even help. He then arranged another 7.5mg of Lupron be given to me and said another petscan is indicated in 3 months. He indicated he was happy with the radiology report which showed my cancer melting away and said they learned a lot from my particular form of prostate cancer. He also indicated I have a hybrid form of cancer, i.e small cell mixed with more normal cancer cells.
9/9/2010-I went to NYC on 9/7 for a lupron injection (7.6mg) and this was a non-event. I met with the doctor and he said my next petscan will be in October. They also drew more blood (CBC, Chem7, PSA) as part of routine testing. No date yet on next visit with the doctor but it will be in October for sure.
9/28/2010-I get my next petscan on 10/12 @ 11am; I then get a lupron injection and meet with the oncologist.
10/9/2010-The petscan was changed to 3pm yesterday so that we could discuss it with the doctor on 10/12 at 12:15pm (saves us a trip to NYC). I have the images from the petscan on a cdrom and my view of them is cancer is still on my right hip and also on my left hip. I await what the radiologist says which I should know Monday (10/11) afternoon. Stay tuned.
10/12/2010-The petscan shows three spots with cancer, both hips and T4 vertebrae. So I signed up for targeted therapy known as LU-J591 which starts in two weeks. LU-J591 means I get an antibody which seeks out cancer and attached to the antibody is a radioactive isotope which then kills the cancer by radiation. I also found out a clinical trial I was in 4 years ago (with Taxotere and Avastin) failed for everyone in it except for me - it didn't help me but at least I didn't die like everyone else! I also received another 7.5mm dose of Lupron and they took 3 more vials of blood and a urine sample and an EKG, all for the LU-J591 therapy pre-screening.
I have been told I am famous among some cancer doctors, mainly due to my rare form of prostate cancer and the fact I have survived 4 1/2 years with it.
10/20/2010-I received a dose (4mg) of zometa along with some saline solution today. Zometa helps protect the bones from metastatic cancer. More details are found by clicking here.
10/27/2010-I had an ingrown toenail on my left foot's big toe. So I went to a podiatrist yesterday who did minor surgery on it and then bandaged me up. He said if it happens again, he has a more permanent solution in mind.
Targeted therapy details are becoming clearer. My first infusion of LUJ591 is 11/11/2010 and then imaging (with gamma camera) on 11/18. The 2nd infusion is on 11/24. Infusion days are generally all day affairs - they give me luj591 and then watch me for side effects for a few hours. I first need a bone scan (and more blood tests) and that happens 11/1. I will be going to the hospital one day a week for a few weeks it seems. They expect me to get chills as a side effect and that is about it.
11/1/2010-The bonescan was uneventful. they gave me technicium 99m and I had to kill 2 hours. So I went to a blood test and then lunch. Then I had the bone scan and then I went home. Technicium 99m has a half life of about 6 hours.
11/4/2010-My neutrophil# is too low for the LUJ591 trial so I had another CBC blood test at Valley Hospital (yesterday) and they faxed it to NYC. It came in at 1.98 (they want 2.0) so I went back again to Valley Hospital today for another CBC blood test. I chose Valley as they are quick about it as opposed to going to a labtech person which could take days.
11/9/2010-We went to NYC to get a blood test and see the doctor. My Neutrophil and other counts are still low. I told the oncologist I had a bad cough some 2-3 weeks ago and had been put on an antibiotic (Levaquin) and he said that is why my counts are low. He said time will bring them back up to normal. The plan now is to get another blood test on Monday and if good, a cat scan on Tuesday and LUJ591 starts the week after. If the count is not good from Monday, I may be put on a new chemo drug (cabazitaxel) along with Neulasta which will boost my counts. The neulasta is a normal part of the chemo drug. I asked about the bone scan, i.e. does technicium 99 get attracted to cancer? The oncologist said the technicium 99 gets attracted to bone activity, bone growing or dying. Cancer can cause that so technicium 99 is a decent marker for cancer.
After all of that discussion, I also received another dose of Lupron (7mg).
11/15/2010-I had another blood test today and this time my neutrophils (ANC) came back at 2.2 so I now am in the LUJ591 targeted therapy program. Next steps include an EKG, a catscan and blood tests tomorrow, getting a port in me on Tuesday 11/23 at 11am and then first dose of LUJ591 is scheduled for 11/24. A week after will be the use of a 'gamma camera' and then a week after the 2nd dose of LUJ591
11/16/2010-I had a cat scan first and I had to drink a cup of this liquid every 10 minutes for an hour before the cat scan, which only took 5 minutes. This liquid 'lights me up' for the cat scan. Then I had blood drawn for PSA and they also wanted a urine sample. Finally, they gave me an EKG for heart function. Busy busy. They said no more CBC blood tests for a while as they have the ANC number they want (2.2) and do not want to chance it going down again. Next on the agenda is getting a port put in me to make blood tests and infusions easier. That is scheduled for 11am on 11/23 and takes about 2 hours - under general anesthesia. You can see a youtube video of the port insertion by clicking here.
11/23/2010-On Tuesday 11/23, I underwent minor surgery to put a port in me. The port is to make infusions far easier and also drawing blood easier. No more finding veins to stick a needle into for this! The surgery lasted 40 minutes and was proceeded by an IV of Vankomycin (an antibiotic) - the IV lasted 1 hour. During surgery I was given Versed to knock me out but I was wide awake through it all, chatting with the surgeon etc.
11/24-I was given 10CC of LUJ-591 through the port and also some saline though the port. They also obtained many vials of blood through the port. After getting LU-J591 (around 110pm), they checked me with a geiger counter and I set it off as expected. I had to stay until 4pm as they watched for side effects (no side effects were observed). I was given an official document (to whom it may concern) stating I was given a radioactive dose, in case I set off some alarms. Next step is imaging and that happens on 12/2. Stay tuned.
12/2-I underwent imaging today. Basically just like a bone scan from a patients point of view for the first imaging. The 2nd imaging was a rotating camera that rotated slowly over 42 minutes. Both looked for radioactivity in me apparently.
12/8-I had my 2nd dose of LUJ-591 and it was a non event- yes it was radioactive like before and I was given it via my port just like on 11/24. We were done by 3pm.
The total doses were 102.6 mCi of 177 Lutetium J591 on 11/11/10 and 11/24/10- for a total of 205 mCi.
1/3/2011-My platelets were 15 last week (it was expected to drop so I received a transfusion of platelets on 12/30. I had an allergic reactions so they get me benadryl. I also had low wbc count so I got a shot of neulasta, also on 12/30.
They measured my platelets again today and now it is 25. My WBC remains low so neulasta has not fully kicked in yet. I am to avoid raw food and unwashed fruit and sick people while my WBC remains depressed.
We go back on Thursday 1/6 at 11am for more blood tests and a possible platelet transfusion again.
1/6/2011-My platelets were 7 today (down from 25 on 1/3) so I got another transfusion of platelets, preceded by hydrocortizone for possible hives.
1/10/2011-My platelets today were 35, up 10 from a week ago. That sounds good. Neulasta (1/3) did nothing for my WBC though - weird!
1/13/2011-My platelets today were 19 but my hemoglobin is down to 9.5 and has been drifting down these last few weeks. So they want to see me again tomorrow and they will retest me.
1/14/2011-I was retested today and my hemoglobin rose by .1 so that is good but my platelets dropped from 19 to 17 so I was given a transfusion of platelets. The transfusion only last 5-8 days (the lifetime of platelets). This is the third round of platelets I have received. I also received 1000 ml of saline as my blood pressure was erratic - at first I felt I did not need the saline but I let them do it anyway,
1/18/2011-They tested me again today and my platelets are at 61 (a new high in recent weeks) but my hemoglobin went down to 9.1 - I get retested in 2 days - stay tuned.
1/21/2011- Platlets are at 52 and hemoglobin remains 9.1 - I opted to get a transfusion of red blood cells to boost the hemoglobin since I get out of breath easily. I received the transfusion today (after a false start yesterday) and now I am not out of breath as often.
1/27/2011-I went to NYC (1/25/2011) to get my blood checked again and platlets drifted down to 39 (from 52) and hemoglobin drifted up from 9.1 to 9.4. I get checked again tomorrow.
2/5/2011-Platelets are now 62 but hemoglobin dropped to 8.9- My oncologist said my low hemoglobin is due to radiation of my pelvis some years ago - I have little reserve left but it should bounce back at some point. I then received a 7.5mg dose of lupron
2/8/2011-Platelets are now 83 and hemoglobin is back to 9.0 - this is good news indeed. My blood chemistry is getting back to normal.
3/8/2011-I was in Florida from 2/10 to 3/6 watching our new granddaughter being born and then came home. While in Florida, I went for weekly blood tests and hemoglobin was low (8.6) and then came back higher (9.9). On 3/8/2011-I was back home and went to NYC and had a catscan, a bone scan and they drew 5 vials of blood and I also received a 7.5ml Lupron shot. today my blood chemistry was a little better (Hemoglobin was 10.2, platelets were 101). A very busy day.
3/10/2011-Ct scan shows cancer likely in lymph glands and T4 section of my backbone. The bone scan shows "Widespread metastatic lesions within the axial and appendicular skeleton". I meet with the oncologist on Tuesday to discuss next steps. It appears the LUJ591 targeted therapy did not work for me although the theory is sound.
3/11/2011-The doctor requested an MRI of my brain today so I went to NYC and had it done. They were kind enough to give me a CDROM of the 345 images of my brain but I cannot interpret it. I see the doctor on 3/15 to discuss next steps (chemo? Clinical trial?).
3/14/2011-The MRI of my brain showed no sign of cancer-hooray! This is good as chemo drugs may not be able to cross the blood-brain barrier and also good as I don't need cancer in my brain. We see the oncologist tomorrow and I have a lot of questions for him related to a clinical trial and/or chemo and which chemo (cabazitaxel?)
3/15/2011-We met with the Oncologist and his team today and they think another clinical trial makes sense. The trial means I get Carboplatin and Paclitaxel as my chemotherapy but in a clinical trial setting. Carboplatin goes after neuroendocrine cancers (Small cell cancers) while paclitaxel goes after adenocarcinomas (prostate cancers). I have both types so I need both drugs. My nurse GinaM then took two samples of blood, assisted by a coworker. GinaM is a great research nurse at a great hospital (NY Presbyterian Cornell Weill Medical Center). I start the clinical trial on 3/17/2011 on which day I get both drugs. Carboplatin is every 4 weeks while Paclitaxel is every week.
3/17/2011-today was a busy day at the hospital - they started by drawing 8 vials of blood (via the port) and then the first round of chemo was given...they started with pepsid then 20mg of zofran and 25mg of benadryl. Then they gave me 183mg of paclitaxol (over an hour) and then 540mg of carboplatin (over a half hour). Then we were done. All infusions came in through my port. I go back in a week but then carboplatin is not given - they skip that for 3 weeks.
3/24/2011-We went to NYC expecting to get paclitaxol but my blood chemistry was too low. Platelets dropped to 50, ANC dropped to 0.8; and RBC was 2.58 so they gave me a 500mcg dose (subcutaneously) of Aranesp to boost my rbc. They asked me to get a CBC blood test on Monday so they could monitor me better. Today's chemo dose was skipped, not postponed and I go for it again on 3/31/2011
3/31/2011-I went to Valley Hospital this past Monday (3/28) and the platelets were 33. I went back to NYC to see the doctor as well as more blood tests. This time the platelets were 31 - too high for a transfusion of platelets (need to be < 10) and too low for chemo to be administered (need to be > 75). So next week is another blood test and the week after is likely more chemo.
3/28 numbers:
RBC 2.30 (s/b 4.4-6)
WBC 1.40 (s/b 4.5-10.5)
Platelets 33 (s/b 150-450)
Hemoglobin 9.1 (s/b 14-18)
ANC 0.64 (s/b 2.03-7.35)
4/6/2011-Went for a blood test yesterday at an local hospital and the results were all low:
RBC 2.37
WBC 1.50
Platelets 34
Hemoglobin 9.3
ANC 0.75
I get another blood test tomorrow per my doctor.
4/10/2011-I went for a blood test on 4/8 and here are the results
RBC 2.32
WBC 1.90
Platelets 27
Hemoglobin 9.1
ANC 0.98
I get another blood test on 4/12 and see the doctor on 4/14 and possibly get some chemo drugs on 4/14. Stay tuned.
04/12/2011-Another blood test today and the results are:
RBC 2.21
WBC 1.60
Platelets 26
Hemoglobin 8.8
ANC 0.75
The counts are still dropping!
4/14/2011-Another CBC blood test today (they took like 9 vials of blood!):
RBC 2.46
WBC 1.6
Platelets 21
Hemoglobin 9.3
ANC 0.8
The other blood was for CMP, Differential and research. The oncologist said he was surprised it was still dropping and perhaps cancer had invaded the bone marrow where blood is made. The only way to say for sure was to biopsy my bone marrow. I agreed with this approach and the doctor said he could do it right there. So I had my bone marrow biopsied (the back of my right hip, above my buttocks). It was painless overall- We should hear the results early next week. He also said to get another CBC test (locally) on Tuesday and we will talk on the phone early next week as to next steps.
4/19/2011-I went to a local hospital for a blood test and here are the results
RBC=2.22
WBC=1.40
PLATELETS=31
HEMOGLOBIN=8.8
ANC=0.50
PLATELETS went up and the others dropped.
4/21/2011-The bone marrow has cancer in it and thus my counts are low. They took blood again tody and then a plan was outlined and my treatment will include Navelbine on a weekly basis (3 weeks on and one week off) and close monitoring during the treatment - thus I am back in NYC on Monday for CBC and likely a transfusion of platelets. Today I did receive 46mg of Navelbine, preceded by 16mg of zofran for nausea control and 12 mg of dexamethazone (a steroid, an anti-inflammatory agent)
Blood test results for today are:
RBC=2.28
WBC=1.3
PLATELETS=28
HEMOGLOBIN=8.8
ANC=.57
4/25/2011-We went back to the hospital for more blood tests and the results are
RBC=2.23
WBC=1.2
PLATELETS=30
HEMOGLOBIN=8.6
ANC=0.5
I also received a dose of 480mcg of Neupogen to boost my WBC; they want me back tomorrow for more of the same (Neupogen). No transfusions for today.
04/26/2011-I went back to the hospital just for a Neupogen shot and then came home.
No blood tests, no tranfusions etc today.
04/28/2011-I had a blood test today and the results are
RBC=2.23
WBC=2.7
PLATELETS=32
HEMOGLOBIN=8.4
ANC=1.65
As you can see the Neupogen injections had the desired effect of boosting my WBC and my ANC counts. We then met with the doctor and his nurse practitioner and the game plan is to get a transfusion of platelets and also of red blood cells and also another injection of Neupogen, all on Monday. After those discussions, I then received 12mg of dexamethazone (a steroid, an anti-inflammatory agent)and 16 mg of zofran (for nausea control) and then 46mg of Navelbine (chemodrug) followed by a short flush with sodium chloride solution.
5/2/2011-I first had a blood test and the results are
RBC=1.97
WBC=1.00
PLATELETS=29
HEMOGLOBIN=7.7
ANC=.66
I then was given 650mg of tylenol, 25mg of benadryl and then 2 units of PRBC (packed red blood cells), each being 350ml. This will boost my RBC and HEMOGLOBIN counts. I was then given 480mcg of Neupogen and I get this again tomorrow. This will boost my ANC and WBC counts.
5/5/2011-today I had chemo (46mg of Navelbine) preceded by 16mg of zofran for nausea control and 12 mg of dexamethazone (a steroid, an anti-inflammatory agent). I also had a blood test and the results are:
RBC=2.84
WBC=1.3
PLATELETS=30
HEMOGLOBIN=9.7
ANC=.40
As you can see, the two units of prbc (red blood cells) bumped my hemoglobin and RBC counts. My WBC stayed up also (2 doses of neupogen did this). My ANC drifted lower though.
5/6/2011-I received 6mg of neulasta in a subcutaneous injection today. I am off from chemo next week but still need to get a CBC blood test mid-week and email it to NYC.
5/11/2011-I had a blood test today and the results are
RBC-2.64
WBC-1.60
PLATELETS-25
HEMOGLOBIN-9.0
ANC-2.08
This showed neulasta had an affect as ANC soared and WBC also went up - this is expected. The other counts are in the same range as prior blood test.
5/17/2011-I had a blood test today and the results are
RBC-2.51
WBC-4.6
PLATELETS-39
HEMOGLOBIN-8.8
ANC-3.03
This showed neulasta had an affect as ANC soared and WBC is normal now - this is expected. The other counts are in the same range as prior blood test.
5/19/2011-I had a blood test today and the results are
RBC-2.57
WBC-4.2
PLATELETS-45
HEMOGLOBIN-8.9
ANC-2.73
Then I got NAVILBLENE as a chemo drug and then one unit of washed red blood cells. I am type A+ and they gave me type O+ (O is universal donor so it is okay). Before all the infusions, I was given 16mg of zofran for nausea control and 12 mg of dexamethazone. I was also given Tylenol and benadryl (to prevent an allergic reaction). Next scheduled events are chemo a week from today and a petscan also.
5/26/2011-This was identical to 5/19/2011 except I had one unit of A+ blood cells and not washed either. I also got a petscan today. Next week is more chemo. I had the usual blood test and the results are:
RBC-2.61
WBC-2.8
PLATELETS-65
HEMOGLOBIN-8.9
ANC-1.9
6/7/2011
We moved to Florida and I received a blood test in Florida. Here are the results
RBC-2.95
WBC-3.1
Platelets-129
Hemoglobin-9.6
ANC-1.8
7/13/2011
We saw the oncologist yesterday and he was happy with the results of abiraterone ( 4 pills all at once on an empty stomach, 1000mg in all). Before I started taking it, I needed one percocet every 4 hours for pain in my chest area. Now I need no pain killers at all so that drug must be working. I also had a CBC blood test yesterday and the results are
RBC-3.26
WBC-3.9
Platelets-135
Hemoglobin-11.3
ANC-2.8
My counts are slowly improving as you can see. They also took a CMP blood test but I do not have those results. They also gave a me a shot of Lupron (7.5mg). We see the oncologist again on 8/11 so no news until likely then.
08/23/2011-I saw the doctor on 8/11 and he was happy with how I feel. I asked if abiraterone worked against small cell cancer and he stated there is no evidence of this. I asked about a petscan and he okayed it. I then received a shop of lupron and then they took blood tests and also flushed both my ports- flushing is needed monthly to prevent clots. Petscan is scheduled for 9/1 at 1030am. I see the doctor again on 9/8. Stay tuned
Blood test results from 8/11:
RBC-3.41
WBC-2.7
Platelets-100
Hemoglobin-11.5
ANC-1.7
08/24/2011-If you have cancer, google these two people
1-Kelley Eidem
2-Johanna Budwig
Both have stumbled on cures for cancer.
I also received an email that one tablespoon of lemon juice (in water) daily has powerful effects against cancer. This was studied by the Institute of Health Sciences, 819 N. L.L.C. Charles Street Baltimore, MD
09/30/2011-I had a petscan on 9/1 and it showed no new growth but PSA is now rising. My wife discovered that getting a dose of zometa (which I did on 9/22/2011 along with lupron on 9/13/2011) can cause PSA to rise for a few weeks. We saw the doctor on 9/27 and he said if PSA is rising because cancer is active again, he will likely do chemo (with Cabazitaxel)....he said a PETSCAN is warranted so that is scheduled tentatively for 10/13. Notice that is far sooner than the normal 3 month wait between petscans- the doctor wants a petscan sooner. The doctor said since I am not symptomatic, he will not rush into chemo and wait on the petscan. I continue to take zytiga (also known as abiraterone) every day as that appears to help in some ways. Stay tuned.
10/13/2011-I get a petscan today and my PSA (from a blood test on 10/11) has risen to 9.1 so I will likely get chemo, outlined above. My platelets were 116 so that is getting better. I also got a shot of lupron (7.5mg) on 10/11. Here are the relevant CBC blood test results from 10/11:
RBC-3.40
WBC-3.2
Platelets-116
Hemoglobin-11.7
ANC-2.1
10/14/2011-The petscan shows all cancers receding to some degree. To quote the report,"Some decrease in the hypermetabolic update associated with previously noted bony metastasis". Good news all around!!
10/14/2011-I received a patient brochure entitled SPEAKUP. I read it and include relevant text from it. It is published by my hospital (we moved to Florida and am now treated at Boca Raton Regional Hospital)
Speak up if you questions, concerns or have something you don't understand. It is your body and you have a right to know what is going on.
Pay attention to the care you are receiving to make sure you are getting the correct treatments and medications. Have medical people treating you washed their hands first? Don't assume anything.
Educate yourself about your diagnosis and medical tests you are undergoing and your treatment plan
Ask a trusted friend or relative to be your advocate, attending meetings with the medical staff, taking notes, asking questions you may not have thought to ask.
Know what medications you are taking and why you take them. Medication errors are very common.
Use a hospital, surgery center or other type of health care organization that has undergone rigorous on-site evaluation against established standards of care, such as those provided by JCAHO.
Participate in all decisions about treatment - you are the center of the health care team. You and your doctor should agree on what exactly will be done at each step of your care. Keep copies of your medical records in case you need to switch doctors and/or hospitals. Don't be afraid to seek a 2nd opinion if you are unsure of what is wrong with you.
11/8/2011
Today I went to see the doctor and also get blood tests, a lupron shot and my ports flushed. It was a nonevent - doctor said I seem healthy and see him again in a month. Below are the results of the CBC blood test:
RBC-3.58
WBC-4.1
PLATELETS-94
HEMOGLOBIN-12.8
ANC-2.8
11/10/2011-My PSA came back at 12.5 so something is going on. My Dr said to stop taking zytiga and wind down the prednisone. He also called my NY doctor to discuss me and said we will talk at next scheduled meeting (12/6)
11/28/2011-I am getting a pain in my left shoulder blade and it requires percocet to calm it down. I started taking a percocet on 11/26/2011. This pain is the same pain I had before I started taking zytiga which they told me to stop taking due to higher psa..
11/29/2011-The Dr ordered two MRIs for me. One of my spine and one of my left shoulder. This was in response to my pain in my left shoulder. The MRI took place tonight @ 745pm. I see him again on 12/6.
12/2/2011-We met with the Radiation Oncologist (Dr MichaelC) and he was very thorough in his exam of me (wiggle my tongue back and forth, press against his outstretched hands, pull his fingers, push against his fingers, raise my eyebrows, squint my eyes, etc etc etc). He was looking for impairment - he found none. I am getting radiation to get rid of the deep throbbing pain in my left shoulder blade which the doctor calls referred pain (not really there but from my spinal cord).We meet again on Tuesday 12/6 at 930am to get prepped for radiation. He also ordered an ultrasound of my left leg to rule out DVT (Deep Vein Thrombosis). This was after he and my wife noticed minor swelling of my left leg. This ultrasound was done today also and no signs of DVT were found.
12/6/2011-busy, busy! We met with the radiation oncology team and based on my history, they plan to use a single dose of stereotactic radiotherapy (STRT) instead of 15 doses on IMRT radiation. I then got a catscan and some tattoos (very small) for mapping purposes. This STRT is scheduled for a few days from now. Between now and then, they want an mri of my thoracic region (mid-back) soon, scheduled for tonight.
Then we saw the oncologist and he was brought up to date by us on radiation approaches and then said I am not symptomatic so no need to rush into anything but he outlined 3 approaches he will take in a months time or so. It includes: chemotherapy (Cabazitaxel), hormone therapy (MDV3100?), more radiation.
We discussed all three approaches and we also found the doctors meet every other week to discuss patients (multi-modality). Then I had my blood drawn again (CBC, CMP, PSA) and my ports flushed and then a lupron shot in my right hip. A petscan will happen after our next meeting in January. Here are my CBC blood tests from today
RBC-3.46
WBC-4.4
PLATELETS-120
HEMOGLOBIN-12.3
ANC-2.6
It will be interesting to see these numbers fluctuate during chemo
12/7/2011
My PSA came back at 17 which means I will start chemo in two weeks or so.
12/8/2011
I am taking up to 4 percocet a day for pain. One around 4pm which is good until 9pm or so. Then another at 10pm so I can sleep without much pain...The pain is now in my right back also but left back is more painful than the right side. It sucks to be me.
On Tuesday they hope to ease the pain with the StereoTactic RadioTherapy (STRT).
12/14/2011-I met with the oncologist and he put me through some neurological tests to see that I am not impaired in any way (I am not). We discussed chemo and it is to start tomorrow. We then got a refill on a prescription for oxycodone (10/325) (as needed for pain but 1 pill every 4 hours is the limir), also for dexmethasone (1 pilll each morning) and then I walked over to where the STRT machine was. They explained it great detail and had me lay down on a table with my arms stretched above my head. They then did a cat-scan to insure I am aligned properly and then the STRT started. Basically you get radiation from 11 different angles, the radiation lasting about 40 seconds each. The radiation piles up where the cancer is and is said to kill it. The hardest part was keeping my arms stretched above my head. They use small tattoos on my chest for alignment and I had my shirt off during all this. Anyway, I was done after the 11 doses of radiation and was told pain and fatigue afterwards are normal for a few days. They gave me a card that had phone numbers to call if I needed to reach them. Then we went home, I am a little tired from all this. I am grateful there are no other side effects, i.e. I could have been paralyzed from the waist down, my esophagus is near that area and that could had affected me eating.....anyway, no side effects - they did a good job with the STRT.
Also for the record, I resumed my anti-cancer diet, i.e. a mix of kale, broccoli, bananas, strawberries, raspberries, habaneros pepper, blackberries, pomegranate juice, blueberries, a carrot, celery.....all put in a blender and chopped up into a thick liquid and then I drink it. I resumed it about a week ago. It worked when I last was on it - it kept cancer at bay for almost a year. So I am trying it again.
12/15/2001-I had chemo and zometa today and just before all these (and supporting drugs), my labs are as follows
RBC-3.02
WBC-3.66
PLATELETS-125
HEMOGLOBIN-10.3
ANC-3.0
Then I received in this order, the following drugs and approximate dosage
o 16mg zofran in saline (anti nausea)
o 25mg benadryl " (anti-hives)
o 10mg decadron " (anti-inflammatory and anti-allergic)
o then a 50 ml flush with saline
o then Cabazitaxel 20mg in saline (chemo drug which also is known as jevtana)
o finally 4mg zometa in saline (helps protect bones)
They also called in tablet form of zofran for use overnight. I expect I will be called back for more CBC cultures over the next few weeks to see how my blood chemistry responds to all the above. Jetvana is known to make one anemic and also deplete platelets so time will tell
12/16/2011-I was very constipated today largely due to eating corn on the cob. lessons learned....anyway I went to bed fully prepared for pain and nausea. I had a bucket by the side of the bed and also took zofran before I went to sleep and had pain meds (percocet) by my bedside. I slept well and no pain meds needed today or zorfan today. Pain is greatly reduced which is good. The unknown now is what jetvana did to my blood chemistry....a cbc blood test will tell and I asked the doctor (via email) when I should come in for a cbc blood test.
12/19/2011-Here are my numbers a few days after chemo. I did not see the doctor, I saw a nurse practitioner instead and she felt I was fine. I told her I was constipated and she said to up colace and also take senna. Here are the blood results:
RBC-2.98, was 3.02
WBC-2.7, was 3.66
PLATELETS-102, was 125
HEMOGLOBIN-10.4, was 10.3
ANC-2.1, was 3.0
12/20/2011-a double dose of colace worked fine...no more constipation.
1/6/2012-On 1/3, I saw the doctor and he said I am doing fine. Then I got a injection of Lupron (monthly). They also took CBC blood tests on 1/3 and here are the results:
RBC-3.25, was 2.98
WBC-3.1, was 2.7
Platelets-125 was 102
Hemoglobin-11.2 was 10.4
ANC 1.4 was 2.1 (notice how ANC dropped)
PSA dropped to 12.5, was 17
On 1/6/2012, I got another dose of chemo. This was preceded by zofran, benadryl, saline and some other drugs. The chemo drug was impaired somewhat to protect my blood chemistry and is known as jetvana (and also called Cabazitaxel).
I went to bed that night and took an oral form of zofran which is good for 8-12 hours it is said. I do not feel nauseous today.
1/13/2012-We met with the oncologist and he said I am in overall good health. They took a cbc blood test and the relevant results are
RBC-2.99, was 3.25
WBC-1.9 was 2.7
PLATELETS-80 was 125
HEMOGLOBIN-10.2 was 11.2
ANC-1.0 was 1.4
PSA-12.1, was 12.5
As you can see, the chemo affected my blood chemistry - this was expected. The next dose of it is on 1/26/2012. After we saw the doctor, I got an infusion of zometa as I was due for that.
01/16/2010-I stumbled upon the concept of nutrient density, i.e. how dense are nutrients in various foods. I was pleasantly surprised to see Kale at the top of the list. Here is the complete list as found on some web pages. Click on it to see it see it more clearly.

1/25/2012-The petscan came back and it was a mixed bag.Some cancers are inactive and some are still quite active, even though I get chemo. The Dr ordered a biopsy to see what kind of cancer I have (small cell? Adenocarcinoma? other?). This is scheduled for 1/31. I also had a blood test which I will post shortly. They also canceled my chemo until they see what kind of cancer I have. Stay tuned.
1/28/2012-Here are the CBC results from 1/25:
RBC-3.27, was 2.99
WBC-2.2 was 2.7
PLATELETS-116, was 80
HEMOGLOBIN-11.1, was 10.2
ANC-1.0 was 1.0 was 1.4
the counts are generally all improved-that is good news.
1/31/2012
I had the biopsy today of the lymph nodes near my aorta. It went smoothly and I should had the results by 2/2....they went in through my middle back with a long needle I guess - I didn't see anything due to being on my stomach. It was CT guided so they took some 6 images to insure they were aiming properly. Afterwards they watched me for an hour and then released me. I asked re why they didn't use ultrasound and they said CT images were clearer. It was not a full body CT scan which is good. Anyway, I had a dull ache in my back for the rest of the day.
2/2/2012-Back at the hospital for a CBC blood test, a lupron shot and a port flush. The biopsy report was not ready yet and the nurse said it can take 5-7 business days for the report. This was a mild shock to us....anyway, we will wait for the report and see the doctor for his plan after the biopsy report is ready. The dull pain in my back is gone but my right leg has a dull pain now---likely due to cancer in my hip bone. I look forward to seeing the doctor. Here are the CBC results:
RBC 3.17, was 3.27
WBC 3.0, was 2.2
Platelets 102, was 116
Hemoglobin 10.5, was 11.1
ANC 1.7, was 1.0
2/6/2012-My oncologist called yesterday (Sunday) and said he spoke with my former NY-based oncologist (Dr DavidN); they agreed to start me on Mitoxantrone and depending how well I tolerate it, also Carboplatin. He also said the biopsy showed simply adenocarcinoma and not small cell cancer. Carboplatin will go after small cell cancer and Mitoxantrone will likely go after both cancers. I see my Boca Raton-based oncologist tomorrow so stay tuned
2/7/2012-We met with the oncologist today and he ordered a MUGA (MUltiple Gated Acquisition scan) REST test for me tomorrow. This noninvasive test measures the hearts function and it's ability. They basically take 3 cc of blood from me, attach Technetium 99 to the red blood cells and inject it back in me. Then they image me to see how well my heart is working. This is because Mitoxantrone (to be given to me on Thursday) is sometimes toxic to the heart muscle. We also interviewed a dentist today and liked what we saw - I wonder - can I get my teeth cleaned if I am getting chemo? I emailed that question to the oncologist. Stay tuned...I will publish the results of the MUGA REST test and also what my oncologist says re teeth cleaning.
2/8/2012-I had the MUGA REST test earlier today. Basically, they get an IV in you and then inject PYP (Stannous Pyrophosphate) which attaches to the red blood cells. Then they take a sample of blood and mix that with Technetium and inject it back in me. It attaches to the PYP. We waited about 20 minutes and then I was imaged. They waited for 600 beats of my heart and then did another image for 500 beats and then I was done. The doctor called late in the day and said my heart was good and not to get teeth cleaned.
2/9/2012-I had chemo today (Mitoxantrone). First they gave me Decadron and then Aloxi (.25mg) and finally Mitoxantrone (27mg). Then they flushed me with 100ml of saline. Mitoxantrone is a beep blue color. Aloxi is an anti-naseau drug and good they say for 3 days. I feel fine afterwards.
CBC results from today
RBC 3.08 was 3.17
WBC 4.5, was 3.0
Platelets 92 was 102
Hemoglobin 10.5, was 10.5
ANC 3.2 was 1.7
2/10/2012-I went to the dentist and they took x-rays and I need dental work but it must be coordinated with the oncologist and also an oral surgeon. Never a dull moment in my life. Anyway, my oncologist will be calling my dentist today. The oncologist at first glance said to do dental work 2 days before chemo or 2 days after. I guess my immune system is strongest then. I also see the oncologist on next Thursday for other reasons.
2/15/2012-I have had a bad cough since Sunday so the doctor ordered a chest x-ray. It turned up nothing of interest. Then we saw the doctor and also had blood drawn for CBC, CMP and PSA. The doctor examined me and then wrote a prescription for levaquin and also cough medicine. He thinks it is an upper respiratory infection. The CMP and PSA blood was drawn through the upper lumen of my port while the CBC was done via a prick of the finger. The CBC results are:
RBC 3.05 was 3.08
WBC 2.1, was 4.5
Platelets 89, was 92
Hemoglobin 10.2, was 10.5
ANC 1.3 was 3.2 (neutrophils)
The lower counts are due to chemo I received last Thursday
2/24/2012-First went to the dentist to consult. I have a bad tooth under a bridge. Due to zometa, I can't have it extracted so a root canal is the likely event. Next step is to remove the bridge and look at the tooth and put a temporary bridge on it. Next, the root canal a week later.
Then we went to the oncologist and we discussed the dental visit and he was a bit surprised about the impact zometa has on dental work. Then he checked me out and I also had three blood draws (CBC, CMP, PSA). The summary from the CBC is below:
RBC 2.80, was 3.05
WBC 1.1, was 2.1
Platelets 47, was 89
Hemoglobin 9.9, was 10.2
ANC 0.3, was 1.3
As you can see, the chemo is knocking my numbers down rather dramatically. This is not unexpected, chemo usually does this to my numbers. I may need a transfusion of platelets in the next week if it keeps dropping. Next week I get more chemo.
2/29/2012-Chemo has been postponed a week as my blood chemistry numbers were still too low. My oncologist also spoke with my dentist and agreed to postpone dental work at least a week. I received a Lupron shot also. CBC today was as follows (slight improvement):
RBC 2.93 was 2.80
WBC 1.9 was 1.1
Platelets 58 was 47
Hemoglobin 10.2 was 9.9
ANC .8 was .3
3/6/2012
Met with oncologist and based on CBC results, he nixed chemo for this week. See below. I also had blood drawn for CMP and PSA and PTT (measures clotting time), Then they gave me 4mg zometa to protect my bones from cancer. I see him again on 3/15.
CBC results:
RBC 2.80, was 2.93
WBC 1.8, was 1.9
Platelets 46, was 58
Hemoglobin 10, was 10.2
ANC .8, was .8
Basically everything drifted down a bit which is why chemo was postponed. The doctor will call me tomorrow with the PSA results.
3/7/2012-The doctor just called and said PSA is 15, down from 18.4. A low PSA is better.
3/15/2012-The doctor saw me and based on CBC results (below), he cleared me for chemo and said to come back tomorrow for a neulasta shot (boosts white blood cells)
Then I received chemo drugs (Aloxi, Decadron, Mitoxantrone-see 2/9/2012 for details) and then we were done. I come back to see him on Tuesday to check my CBC again. Here is todays CBC:
RBC 2.74, was 2.80
WBC 2.3, was 1.8
Platelets 63, was 46
Hemoglobin 9.8, was 10
ANC 1.1 was .8
03/27/2012-We went to the see the doctor today and to get blood tested. I had CBC, CMP and PSA tested. The CBC results are
RBC 2.43, was 2.74
WBC 2.8, was 2.3(Neulasta accounts for the increase)
Platelets 19, was 63 (chemo did this to me)
Hemoglobin 8.6, was 9.8
ANC 1.6 was 1.1 (Neulasta accounts for the increase)
I also received a dose (7.5mg) of lupron via an injection. The doctor pronounced my lungs very clear and I said I still had the cough. He put me on a special steroid for 5 days and said that should make the cough go away. He asked we see him again in a week. Re low platelet count, he said to use an electric razor and not a blade razor for future shaving. The Doctor called the next day (3/28) and said my PSA continues to go down and is now 13 (was 15 and before that 18). CMP was all fine per the doctor.
4/3/2012-My CBC chemistry was still too low for chemo but I did receive 4mg of zometa today. My CBC was:
RBC 2.35 was 2.43
WBC 2.9 was 2.8
Platelets 39 was 19
Hemoglobin 8.4 was 8.6
ANC 1.8 was 1.6
The plan is for chemo next week if my platelets continue to rise.
4/10/2012-We saw the oncologist and he sent me for a chest xray to see what is causing my cough. We went home after all that.
4/13/2012-A lot has happened. I woke up Wednesday (4/11) with 100.5 fever. We called the on-call team at the hospital and they said to go to the ER. We did this and they found my hemoglobin (from a blood test) was very low (6). I also had a bad cough.
They admitted me quickly and then gave me two units of blood to boost my hemoglobin count. This ended at 12:10am (Thursday 4/12)) so I went to sleep (in room 801). The next day they scheduled a cat scan to see if any thing going on. Nothing found. They collected my fecal matter and no blood found in them. They gave me oral treatment for the cough (breath in medicine across a long tube) every 5 hours or so. They gave me steroids also (via my port). They constantly drew blood to monitor my blood chemistry levels. My oncologist dispatched a cough specialist to see why I was coughing (bronchitis). Friday (today), I feel better and nothing else was found except for anemia and bronchitis...so they sent me home. The hospital was Boca Raton Community Hospital...a good hospital. Here is CBC results from 4am this morning, after transfusions etc
RBC 2.85 was 2.35
WBC 2.7 was 2.9
Platelets 46 was 39
Hemoglobin 9.9 was 8.4
ANC not available
4/17/2012-We saw the oncologist today and he said I look healthy but no chemo this week-he said to give it another week to allow my counts become normal...so next week instead. He discussed my current CBC results and they were good:
RBC 3.02 was 2.85
WBC 4.3 was 2.7 (normal!)
Platelets 70, was 46
Hemoglobin 10.5 was 9.9
ANC 3.4 (normal!)
I had been wearing a mask when I go out but I need not do that anymore as my WBC#s are what protects me from infections etc....the WBC is normal now
4/18/2012-I emailed the oncologist, asking if I can take 81mg aspirin. He replied it was okay. That is good as aspirin prevents blood clots. He replied yes in light of my improved blood chemistry. He also called me and said PSA was down to 10.
4/25/2012-I went to see the oncologist yesterday and he said I am in good shape to get chemo today which I did. Here are the CBC numbers from yesterday
RBC-2.78 was 3.02
WBC-3.2 was 4.3
Platelets-80 was 70
Hemoglobin 9.8 was 10.5
ANC-2.2 was 3.4
I did receive chemo today, first decadron (10mg), a steroid. Then an anti-nausea drug Aloxi and then Mitoxantrone 13.5mg, followed by a flush to insure I received it all. I also received a dose of Lupron which I get monthly.
4/26/2012-Received a shot of neulasta to boost the WBC number. The next CBC will show the effect of neulasta.
5/2/2012-I had a petscan yesterday and saw the doctor today. Based on the petscan, I have two types of cancer and one is dying from the chemo but the other is small cell and still doing fine. My oncologist said he would contact my NY doctor to discuss next steps which will likely include a platinum based chemo at a reduced level. The CBC levels are:
RBC 2.68, was 2.78
WBC 0.9 was 3.22 (soon to rise due to neulasta effects)
Platelets 34, was 80
Hemoglobin 9.1 was 9.8
ANC was 0.3 was 2.2 (soon to rise due to neulasta effects)
I got a dose of zometa today (prior was 4/3! too soon?) and they also took blood for CMP and PSA.
5/3/2012-The doctor called and said monthly zometa is okay and my PSA is now 14.5
5/9/2012-Met with oncologist today and he had not heard back yet from my NY oncologist. My FL oncologist who I met with today is inclined to go with a platinum-based chemo drug to battle the small cell cancer. My counts are still too low so we agreed to meet again next week. My CBC results are:
RBC 2.58 was 2.68
WBC 3.3 was 0.9
Platelets 24, was 34
Hemoglobin 8.8 was 9.1
ANC 2.3, was 0.3
5/15/2012-Went to see the nurse practitioner (doctor was on vacation). She showed me my CBC and said I need a blood transfusion (2 units) to boost my hemoglobin. So they drew more blood (for type and cross as prelim to transfusion). CBC results are:
RBC 2.12 was 2.58
WBC 2.6 was 3.3
Platelets 27 was 24
Hemoglobin 7.6 was 8.8
ANC 1.7 was 2.3
5/16/2012-I had the blood transfusion today - 2 units of A+ blood. This was done to boost my hemoglobin count which was dangerously low and I was getting lightheaded from the low count.
5/22/2012-Met with Oncologist today and we have a plan, developed jointly between my FL Oncologist and my NY Oncologist. I will be given Cisplatin and VP16 (known also as etoposide) at a reduced level but more often. We will watch my blood CBC levels as we go along in this process; I also had CBC blood levels checked today and they are low so the planned chemo starts tentatively next week. I also got a shot of Lupron. CBC levels follow:
RBC 2.88, was 2.12
WBC 2.9, was 2.6
PLATELETS 39, was 27
HEMOGLOBIN 9.6, was 7.6
ANC 1.6, was 1.7
5/30/2012-Met with oncologist and he said, based on CBC blood chemistry, he wants to wait another week for chemo so that is scheduled for a day next week. My CBC results are:
RBC 2.87, was 2.88
WBC 2.1, was 2.9
Platelets 55, was 39
Hemoglobin 9.6 unchanged
ANC 1.3, was 1.6
6/07/2012-Met with oncologist and, based on CBC results, he cleared me for chemo. The sequence of chemo drugs given was:
Dexamethazone (a steroid)
Aloxi (anti nausea drug good for 72 hours)
Saline flush
Potassium (1 hour infusion)
etoposide (2 hour infusion-reduced dosage, approx 25% of normal)
saline flush
cisplatin (2 hour infusion-reduced dosage, approx 25% of normal)
saline flush
My CBC results were:
RBC 2.76, was 2.87
WBC 2.6 was 2.1
Platelets 63, was 55
Hemoglobin 9.5 was 9.6
ANC 1.4 was 1.3
The plan calls for weekly chemos and weekly CBC blood tests
6/14/2012-My CBC blood test was yesterday and results are below. I was cleared for chemo so I got that today and it was the same regimen as 6/7/2012 (above). I also developed thrush in my mouth so I take pills for that and it is clearing up - prednisone makes you predisposed to getting thrush. I found out cisplatin tends to clear the body of potassium so that is why they gave me a potassium infusion.
The CBC results are:
RBC 2.59 was 2.76
WBC 2.9 was 2.6
Platelets 67 was 63
Hemoglobin 9.0 was 9.5
ANC 1.6 was 1.4
6/21/2012-I had chemo today as well as blood draws for CMP and PSA. I also had a lupron shot. See 6/7/2012 for details on the chemo received today. I had CBC blood test yesterday and results are
RBC 2.55 was 2.59
WBC 2.7 was 2.9
Platelets 59 was 67
Hemoglobin 9.2 was 9.0
ANC 1.4 was 1.6
6/28/2012-I had chemo today. See 6/7/2012 (above) for details.
7/3/2012-I had a CBC blood test today (results below) and a CMP blood test (to test magnesium levels):
RBC 2.42 was 2.55
WBC 2.2 was 2.7
Platelets 52 was 59
Hemoglobin 9.4 was 9.2
ANC 1.3 was 1.4
7/5/2012-I had chemo today (see 6/7/2012) and also zometa. CMP came back and magnesium was a bit high. Not a cause for concern.
7/12/2012-My counts are too low for chemo so the doctor said wait a week. The counts that are low include WBC, RBC, Hemoglobin and Platelets. The chemo I received for the last 5 weeks knocked them down. I was told to watch for cuts and a fever and go to the hospital if I get either.
RBC 2.35 was 2.42
WBC 1.8 was 2.2
Platelets 38 was 59
Hemoglobin 8.7 was 9.4
ANC .9 was 1.3
7/18/2012-Counts are still low so no chemo this week. My SO mentioned I am "loopy" in the evening and the doctor ordered an MRI of my brain and also a petscan of my body (I am due-every 3 months and last was 5/1). CBC results are:
RBC 2.43 was 2.35
WBC 1.2 was 1.8
Platelets 37 was 38
Hemoglobin 9.3 was 8.7
ANC .3 was .9
7/25/2012-Yesterday, I had an MRI of my brain (no problems found), a petscan of my whole body and no material change since 5/1's petscan. I had a CBC blood test today and the oncologist said to get chemo tomorrow and see him in 2 weeks. He expects chemo to knock my counts down a bit and then they should rebound. Below are my CBC counts as of today:
RBC 2.36 was 2.43
WBC 1.9 was 1.2
Platelets 36 was 37
Hemoglobin 9.1 was 93
ANC 0.2 was 0.3
7/26/2012I had chemo today....see 6/7 for details on what I get....it started at 10am and ended around 2:30pm - a long day....I felt shitty the rest of the day and I took a pill for anti-nausea effects. I felt better on 7/27/2012.
8/9/2012-I had chemo again today.....see 6/7 for details on what I get. It started at 9:15 and ended around 2pm. Here are CBC results from yesterday. No chemo scheduled for about2 weeks, depending on CBC results:
RBC 2.36, was 2.36
WBC 2.0, was 1.9
Platelets 40, was 36
Hemoglobin 8.8 was 9.1
ANC .9 was .2
08/22/2012-I had a CBC blood test today along with a CMP and PSA blood test. The CBC results are below. We decided to postpone chemo into next week as counts will be higher then. Here are the CBC results:
RBC-2.21, was 2.36
WBC 2.4, was 2.0
Platelets 49, was 40
Hemoglobin 8.8 was 8.8
ANC 0.6 was 0.9
09/08/12-We went on a trip back to the northeast and visited Vermont and Pennsylvania and NJ. We also visited with my NY oncologist on 8/28/2012 who ran various blood tests:
RBC 2.1,was 2.21
WBC 2.4 was 2.4
Platelets 53 was 49
Hemoglobin 8.7 was 8.8
ANC 0.7 was 0.6
PSA 24.5
9/11/2012-My FL oncologist will suspend my cisplatin/etoposide chemo and put me on a new drug (approved by FDA on 8/31/2012) known as MDV3100 (an oral drug, also known as enzalutamide). I had both lumens in my port flushed today. I had CBC, CMP and PSA blood tests today also and the CBC results are:
RBC 2.46 was 2.1
WBC 2.9 was 2.4
Platelets 60, was 53
Hemoglobin 9.7, was 8.7
ANC-1.7 was 0.7
PSA was 23.
10/1/2012-MDV3100 arrived on 9/28/2012 and I commenced taking it that day. 4 pills a day with or without food.
10/2/2012-I went to see the doctor today and they took blood tests (CBC, CMP, PSA) and also an x-ray of my right leg (femur). This is because I have a dull pain in that part of my body and I am taking Alleve for it. The CBC results are:
RBC-2.4 was 2.46
WBC-3.2 was 2.9
Platelets-70 was 60
Hemoglobin-9.5 was 9.7
ANC-1.2 was 1.7
10/25/2012-I continue to take MDV3100 (aka XTANDI, 4 pills a day) and today I received zometa via my port (top lumen) and also a CBC Blood test was taken:
RBC-2.76, was 2.4
WBC-3.0 was 3.2
Platelets-71, was 70
Hemoglobin-10.3, was 9.5
ANC-1.3 was 1.2
11/8/2012-I continue to take XTANDI. I developed a dull pain in my right leg. X-rays the same day showed nothing. I also received a shot of lupron and they also took blood for CBC,CMP and PSA:
RBC 2.66, was 2.76
WBC 3.2, was 3.0
PLATELETS 60, was 71
Hemoglobin 10, was 10.3
ANC 1.6, was 1.3
PSA 34, was 23 a few weeks back.
11/19/2012-I had a petscan on 11/15/2012 and it showed cancer has "signficantly worsened" in me. It is on my ribs, my sternum, my hips etc. The doctor canceled XTANDI (it didn't work) and will soon start me on Cytoxan and vincristine.
11/21/2012-I had chemo today. First was Aloxi for nausea control and then some other drugs to enhance aloxi. Then I was given cytoxan and Vincristine, apparently in small doses. I felt weird all day from these two drugs and am to watch for side effects and also drink 2-3 quarts of water per day.
11/28/2012-I met with he oncologist and had a CBC blood test. The doctor said I had a reduced level of chemo last week and my blood chemistry is largely unchanged. If it stays that way next week, I will get more chemo next week. Here are the CBC results:
RBC-2.71 was 2.66
WBC-2.1 was 3.2
Platelets-60, unchanged
ANC-0.8, was 1.6
12/4/2012-I met with the oncologist and he said my counts are lower so no chemo tomorrow. I explained my right leg hurt and I needed oxycodon for it. He scheduled an MRI of my spine as the xrays of the leg showed nothing.
CBC results:
RBC-2.66 was 2.71
WBC-1.7 was 2.1
Platelets-68, was 60
Hemoglobin-9.4, was 10
ANC-0.6 was 0.8
PSA-43
The MRI showed no cancer in my brain and provided additional details on the cancer on my bones.
12/11/12-We met with the radition oncologist and he proposed a series of radiation treatments to kill the cancer hurting my right leg. He also proposed a set of treatments high on my spinal cord and said 1 out of 1000 men develop sore throats from it. I am inclined to go for that treatment also. Treatment for leg pain starts soion.
12/19/2012-The pain my leg spread to my right foot and required two 10/325 oxycodon pills every 4 hours to keep the pain at bay. We met with a nurse in radiation oncology and asked for a 25 mcg Fentanyl (an opiate narcotic) (a transdermal patch) as a better pain killer. Once the fentanyl kicked in I was down to 1 oxycodon every 6 hours. I had my second dose of radiation today and it takes a total of 15 minutes to administer.
12/20/2012-I had my 3rd dose of radiation and then FOUR blood tests. They also flushed both lumens in my port. The FOUR blood tests include CBC, CMP, PSA and Lipid Panel (which I needed to fast for). I had taken gemfibrizol about an hour before and that tweaks my trigricerides count down. The CBC results were
RBC 2.59, was 2.68
WBC 2.2 was 1.7
Platelets 58 was 68
Hemoglobin 9.3 was 9.4
ANC 1.3 was 0.6
01/03/2012-After the 4th radiation dose, I developed a bad sore throat. We met with the radiation oncologist after the 5th dose and he doubled by fentanyl to 50mcg. The pain in my leg is gone - good news. I am at my 10th dose now and have switched to a liquid diet (smoothies, Ensure, jello, soup, etc) due to the sore throat. They also gave me fliers on what to do for a sore throat, constipation etc.
01/08/2012-I have one more radiation dose to go. I need to take 2-3 Ocxycodons daily to keep pain down even thought I have a 50mcg Fenatnyl. The oncologist said he would talk about my pain in my left shoulder/arm to the radiation oncologist to see what can be done. I then had both ports flushed and and they drew blood for CBC, CMP and PSA. I also got a 7.5mg shot of lupron
I will post relevant CBC tomorrow.
01/10/2012-I didn't get the CBC results but the doctor called and said my PSA is now 50 and he will start me on Taxotere (at a reduced dose level) next week. Taxotere makes sense as that form of cancer expresses PSA while small cell cancer does not. Stay tuned. As of today, my throat hurts (from 35 grey units of direct radiation), my left arm hurts (from radiation). I take oxycodon (10.325) 3 times per day for the pain and also use a Fentanyl (10mcg) patch. It is tough being me.
01/13/2012-Went to a local ER due to pain in my left shoulder area. It was like a stabbing pain. The ER did blood test, EKG and an X-ray. They said no problem found but my heart looks fine (they suspected a heart attack I think). They sent us home about 2 hours after we got there and said to continue pain meds as needed. The CBC from the ER visit is shown below: RBC 2.33, was 2.59
WBC 1.7, was 2.2
Platelets 61 was 58
Hemoglobin 8.3 was 8.3
ANC not available
01/17/2013-Saw the oncologist 2 days ago and he said I was greenlighted for chemo. I would get a reduced dose (of Taxotere) every 2 weeks. The CBC from today is RBC 2.86, was 2.33
WBC 2.4 was 1.7
Platelets 67 was 61
Hemoglobin 9.0 was 8.3
ANC 0.9 was 1.3
01/17/2013-Yesterday I had severe pains in my left and right front rib cage. Required Oxycodone to take the edge off the pain.
01/17/2013-Today I received a reduced dose of taxotere after getting zofran. It was uneventful. Next dose is in about 2 weeks or so, depending on blood chemistry. My PSA dropped again to 31.
02/1/2013-I went for radiation to stop the pain in my left rib cage. This is still ongoing. They took my blood tests and noticed my hemoglobin is low so I received (1/31) 2 units of A+ blood over the course of 4 hours. The top lumen of my port was stop and go so so they switched to the bottom lumen and that worked much better; here are the CBC results from yesterday
RBC 2.26, was 2.85
WBC 1.4, was 2.4
Platelets 41, was 67
Hemoglobin 7.8, was 8.3 (This triggered the transfusion)
ANC 0.9 was 0.9
PSA 31
2/4/2013-Much has happened....We went to the beach yesterday. My Friend Phil helped me to my feet and I promptly blacked out.My wife helped Phil get me to my feet and I was fine again. She called the doctor and he said to come on and get my blood levels checked. The Nurse Practitioner noticed I was unsteady on my feet and ordered a wheelchair for me. I see the doctor again tomorrow and also get 3 MRIs.
2/5/2013-Joe was rushed to the ER shortly after midnight...we was unable to stand.
2/10/2013-I've been in the hospital for about a week. After I received my 3 MRIs, the doctors determined that there is cancer in my spine causing a spinal cord compression - leaving me unable to walk. I received a 4th MRI earlier this week of my brain which was clear. I received radiation of my ribs to relieve pain. At the moment, I am in BRCH. Plans call for me to go to hospice in the future.
2/11/2013-My name is Marilyn. I am Joe's wife. Joe is unable to update the blog at this time so I will type for him. Joe was transferred to Hospice by the Sea today. It was a very difficult transition to hospice care. As you know, Joe has been a real fighter in this battle. We have had to move from fighter mode to comfort mode.
The MRIs revealed that cancer has invaded each vertebrae in Joe's spine. There is a compression fracture in T4 and cord compressions in the lower spine. Joe is no longer able to stand or walk. There was a neuro-surgical consult in the hospital to see if surgery could relieve the pain. It was determined that Joe's blood levels were too low for surgery and the out come would not improve his situation.
The palliative care oncologist told me today that Joe has only a few days left. Since we just met him, I called in his regular oncologist to see if he concurred. Knowing Joe and Joe's determination to beat this horrible disease, he determined that Joe still has more that a few days.
2/14/2013-Joe, the energizer bunny, has yet again, fooled the experts. With the help of many meds, he is stable and comfortable and there is talk of sending him home for in home hospice care.
2/15/2013-Joe had a blood test today. He was pale and lethargic.
2/16/2013-Blood test revealed that Joe's hemoglobin has lowered a bit but is not low enough for a transfusion. Joe is confused and in and out of sleep.
2/20/2013-Joe had another blood test. Results revealed lowering hemoglobin, WBC and platelets. We are afraid he is again on a downward spiral.
2/24/2013-A blood test was done again today. Hemoglobin was 8.1, platelets are 28 and WBC is 2.0. Blood transfusion was ordered and administered at night.
2/25/2013-Joe is once again back with us. More talk of sending Joe home. Hospice care is amazing. Oncology and hospice nurses are angels...this line of work is not a job. It is a "calling".
2/28/2013-Joe came home from hospice today. He was grinning from ear to ear. Hospice had delivered a hospital bed, tray and oxygen generator. Joe was transferred to the bed and slept most of the remainder of the day. The travel exhausted him. We have hired 24/7 caregivers to assist with his care. He needs to be turned in the bed every few hours to prevent bed sores. They will also tend to his other needs. He is now completely incontinent.
3/3/2013-Joe not doing very well today. Not eating very much.
3/4/2013-Joe had a horrible night last night. Vomiting and diarrhea for hours. Had a fever of 101.5. Hospice nurse was called in and she gave Joe some meds to help him through this crisis. Today he is very lethargic. He has only eaten a slice of dry toast and some chicken soup. His stomach is enormous and he is sweating profusely. Many caring family members are present to help with his care and comfort him. We wonder if he will make it through the night.
3/5/2013-I awoke this morning to the door bell ringing. The shift change of caregivers was occurring. As I walked past Joe's bedroom door to answer the door, I saw Joe sitting up and smiling! His cheeks were rosy and he was watching TV. After letting the day nurse in, I went back to him and he asked me for a cup of coffee and some breakfast! He wants me to order a wheel chair and scooter! He tried to pull himself up with the side rails of the bed.
3/7/2013-Joe was very sleepy today...not much of an appetite. Urine in bag became increasingly bloody. Phoned Hospice nurse in early evening. He changed catheter and ordered some meds. Joe had a mild fever. While hospice nurse was there, family and friends cooked dinner. When Joe smelled it, he perked up and wanted to eat some meatballs, one of his favotite foods. He ate several, followed by vanilla ice cream and was off to dreamland.
3/8/2013-I woke up to some commotion in Joe's room. The aide was bathing Joe for the day and Joe was feeling nauseous. I started helping the aide and Joe began to vomit. He was lethargic, urine was extremely bloody. Called hospice and they again, sent a nurse. Joe was moved back to Hospice facility shortly after. Once at Hospice, continuous bladder irrigation was started. Joe slept all day, ate nothing.
3/9/2013-Joe was wide awake in the morning; he ate 1/2 slice of toast and some OJ. Our friend, Phil, left and Joe's aunt and uncle arrived from VA for a short visit. He ate 2 bites of a grilled cheese for lunch and fell asleep for rest of day. Little urine output but normal color finally.
3/12/2013-Joe was awake until about 3pm; he ate a piece of grilled cheese. He got mildly nauseous and had some mild pain in stomach, no doubt from not eating very much. Wet cough developed. Got some meds for the cough.
3/13/2103-Joe slept from about 8 last night until 6pm this evening. Nurse confided to me that she felt he is declining. When he woke he was quite peppy, ate a whole grilled cheese (this is one of his favorites, by the way). I could barely make out what he was saying when he spoke...speech quite garbled. He needed some additional pain meds for back pain. Had breathing treatments for cough.
3/14/2013-Joe was awake when I arrived at hospice. He had already eaten some toast and Cheerios for breakfast. He was very confused and disoriented...kept asking for a green blanket and wanted to know why I wasn't at work (I haven't worked for 2 years)...also spoke about people he has not seen in 20-30 years. He fell asleep at 11am. During the afternoon, he was given some meds for some agitation. He slept until the next morning.
3/15/2013-When I arrived at Hospice, Joe was awake and his breakfast tray was there but cold. I heated it up and he ate a couple bites of toast, some thickened OJ and some water. Joe then fell asleep again. He even slept through the doctor's visit. Doctor said Joe is continuing to decline. At lunchtime, I left Joe to run some errands and when I returned just before 2pm, I found Joe noticeably agitated. He was clawing at his hospital gown and actually pulled it off. He tried to pull out his port access and his catheter. He threw off all sheets and blankets. I must have put his gown back on 10 times before I realized it was a loosing battle.
The nurses gave him something for the agitation and when that didn't work, they tried something else. There was just nothing to ease his discomfort. He was staring to moan by now, but when I asked him if he was in pain, he shook his head "no". He was not able to take his nerve pain meds for two days because he could not swallow them (guess there is no liquid version). I left for dinner at 7:30 and when I returned at 9, a morphine pump had been started. Joe looked comfy but he was still moaning. No matter what I said to him, he could not stop. My heart is so heavy...
3/16/2013-Joe is still moaning when I arrive at hospice. I called for the nurse and he was moved to a more comfortable position and his pain meds were adjusted. We realized at this point that Joe is in much pain when he is on his back. The doctor stated that Joe's passing is "imminent". He is still sleeping and is not eating. He remains comfortable for the rest of the day.
3/17/2013-Joe is still sleeping, not eating. His breathing becomes more and more labored. His blood pressure falls throughout the day. The nurse says the end of Joe's life is near. At about 9pm, I sent our son and his wife and my brother home. I made up the bed in Joe's room so that I could stay with him. The nurses came in to move Joe and while we were doing so, one of the nurses asked me how Joe and I met. I related the story to her and as I finished, I noticed Joe's eyes opening. I went to his side and he opened his eyes, gasped for breath and stopped breathing, he did this two more times and then stopped breathing. It was about 9:50pm. His eyes closed for the final time. Joe's journey had ended. My brave, beautiful man is finally disease and pain free again.
If you would like to create a memorial for Joe or to support prostate cancer research, please send donations to: Weill Cornell Medical College, Prostate Cancer Research, c/o Dr. David Nanus, 1305 York Ave., 7th Floor, New York, NY 10021
We welcome your comments on this blog. Please email by clicking here: marcollins3040@gmail.com

Labels: prostate cancer diary
